Prescribing & Prescribing Assessment
Bradford VTS Clinical Resources
- by Dr Ramesh Mehay & Sabah Malik
- Last modified: 3rd February 2024
- No Comments
DOWNLOADS
path: PRESCRIBING
- prescribing-analysis-tools
- 10 tips for safer prescribing.pdf
- analgesia prescribing rationale.doc
- antibiotic coping strategies.pdf
- antibiotic prescribing by PACE bradford.pdf
- antibiotic prescribing.doc
- antibiotics – long term prophylaxis for uti.docx
- anticholinergic drug problem.pdf
- computerised prescribing.doc
- coping with drug side effects.rtf
- cumulative drug toxicity tool for elderly.pdf
- deprescribing antipsychotics in elderly.pdf
- deprescribing benzodiazepines and z drugs in elderly.pdf
- doctors bag – ashcroft 2021.docx
- doctors bag.docx
- dont prescribe these.doc
- drug and vaccine trials and phases.docx
- drug efficacy and NNT.pdf
- drug efficacy NNT table.pdf
- drugs to review – special notes on specific drugs.pdf
- frailty & short life expectancy – identifying.pdf
- health economic analysis of polypharmacy.pdf
- high risk medications for causing errors.pdf
- medication and falls in elderly.pdf
- medication in the frailest adults.pdf
- medication review – 7 steps.pdf
- medication review framework – detailed.pdf
- medication review framework – simple1.pdf
- medication review framework – simple2.pdf
- medication safety.pdf
- medications that are high risk for causing errors.pdf
- mrcgp – prescribing errors and suboptimal prescribing – the PRACtICe study and 100 prescription study.docx
- nocebo effect – example with statins and antidepressants.docx
- nurse prescribing.doc
- opioid conversion chart 2021.pptx
- oxygen equipment guide.pdf
- phamaceutical companies – how tainted is medicine.doc
- pharmaceutical companies and the media.ppt
- pharmaceuticals industry (with slide notes).ppt
- polypharmacy guidance and realistic prescribing manual 2018 – scotland 3rd edition – excellent.pdf
- polypharmacy.pdf
- population vs personal medicine – a story after candide.doc
- practical prescribing – good guidelines.doc
- practical prescribing – medication reviews and repeats.pdf
- practical prescribing – prescription queries.doc
- practical prescribing – repeats acutes dossets.doc
- practice formularies.pdf
- prescribing – sick day rules for elderly.pdf
- prescribing abbreviations and symbols that cause errors.pdf
- prescribing book – chapter 0.pdf
- prescribing book – chapter 1.pdf
- prescribing book – chapter 2.pdf
- prescribing book – chapter 3.pdf
- prescribing book – chapter 4.pdf
- prescribing book – chapter 5.pdf
- prescribing in children.pdf
- prescribing tutorial on 2 sides of A4 (TEACHING RESOURCE).doc
- prescription charges – who pays who doesnt.doc
- prescription writing exercise (TEACHING RESOURCE).doc
- prioritising patients for medication review – potential projects.pdf
- qt prolongation with psychotropic medication – what to do.pdf
- smoking cessation – the clinical bits.docx
- steroid therapy induced hyperglycaemia – management.pdf
- warfarin to doac switching guide.docx
WEBLINKS
QUICKLINKS
PATIENT LINKS
……………………………………..
Information provided on this medical website is intended for educational purposes only and may contain errors or inaccuracies. We do not assume responsibility for any actions taken based on the information presented here. Users are strongly advised to consult reliable medical sources and healthcare professionals for accurate and personalised guidance – especially with protocols, guidelines and doses.
COME AND WORK WITH ME… If you’d like to contribute or enhance this resource, simply send an email to rameshmehay@googlemail.co.uk. We welcome collaboration to improve GP training on the UK’s leading website, Bradford VTS. If you’re interested in a more active role with www.bradfordvts.co.uk (and get your name published), please feel free to reach out. We love hearing from people who want to give.
……………………………………..
ELEMENTOR TEAM - can play with this tabs widget
Elementor team. Play with this widget and see how slow it is on every page. Try to
- make a duplicate of the widget = takes forever
- move four of the tabs around = takes forever and then holds!
- delete four of the tabs = takes forever.
This site is for doctors and many doctors around the world rely on it. It provides free medical information and so it is important that this site runs smoothly. But some of my very small team wont now use it to update the website because they say it is so incredibly slow. Please help so we can continue supporting doctors around the world.
Many thanks
Dr Ramesh Mehay
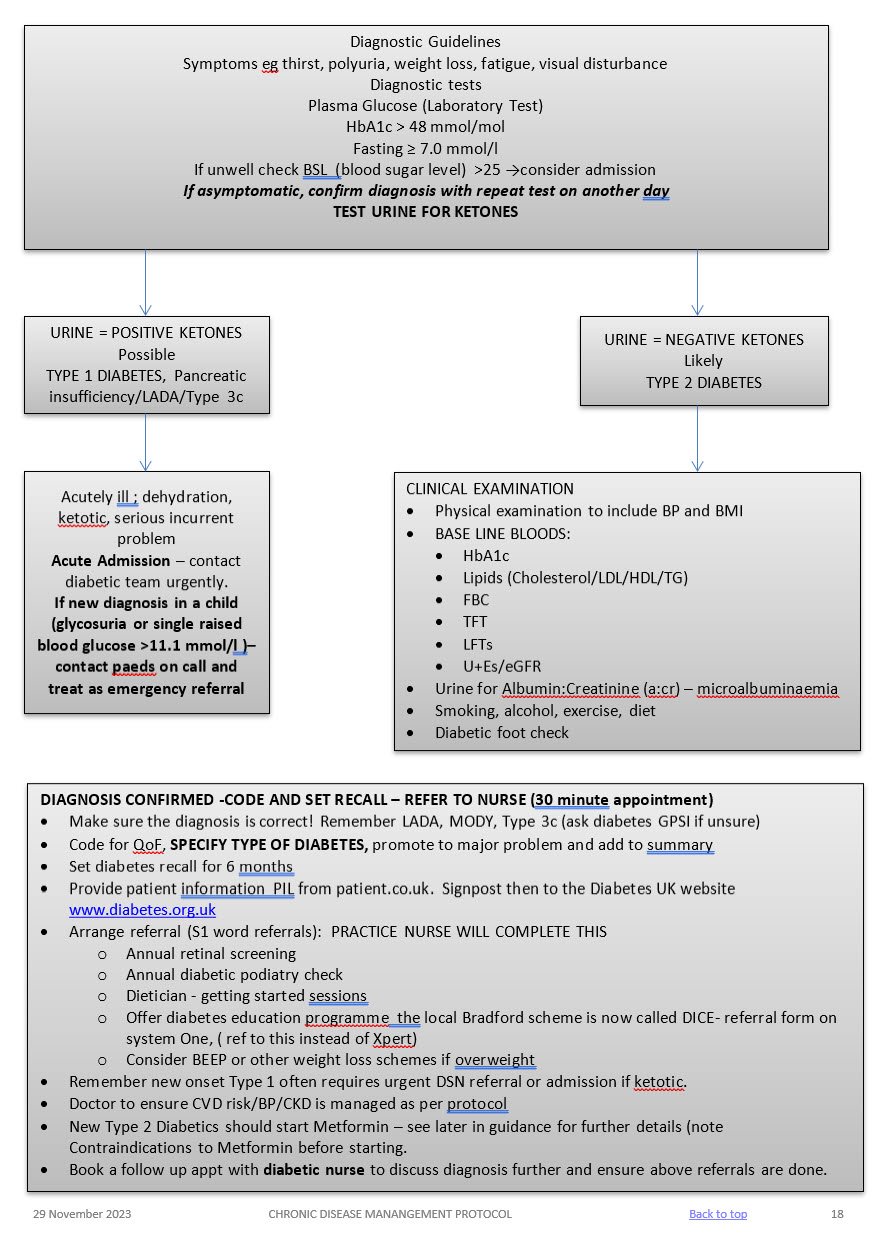
SYMPTOMATIC
Symptoms of hyperglycaemia (polyuria /polydipsia, unexplained weight loss. visual blurring, genital thrush, lethargy) plus either:
HbA1c: 48mmol/mol or higher (LAB TESTING) (Type 2 diabetes is diagnosed in adults who are not pregnant and do not have haemoglobinopathy or haemolytic anaemia by a glycated haemoglobin (HbA1c) level of 48 mmol/mol or above.
The WHO state that diagnosis should be confirmed with a repeat HbA1c test, unless clinical symptoms and plasma glucose levels >11.1mmol/l are present in which case further testing is not required.)
FBG: >7.0mmol/L or higher x2
Dip urine to check for ketones
ASYMPTOMATIC
In the absence of symptoms – 2 abnormal results on separate days are required for the diagnosis.
Results:
- HbA1c > 48 mmol/l → repeat HbA1c test after 2 weeks → if HbA1c >48 mmol/l then code Diabetes and set recall
- HbA1c 42-47 mmol/l → code and set “at risk of diabetes” recall
May not be accurate in the following cases:
- ALL symptomatic children and young people
- Symptoms suggesting Type 1 diabetes/pancreatic insufficiency (any age)
- Short duration diabetes symptoms
- Patient at high risk of diabetes who are acutely ill
- Taking medication that may cause a rapid glucose rise e.g steroids, antipsychotics
- Acute pancreatic damage/pancreatic surgery
Patients with haemoglobinopathy – the labs test for this and will detect abnormalities.
A diagnosis of diabetes has important legal and medical implications for the patient and it is therefore essential to be secure in the diagnosis.
A diagnosis should never be made on the basis of glycosuria.
A stick reading of finger prick should be confirmed by a venous sample, as per NICE guidelines.
What is it?
When we mention the cytochrome P450 system, most doctors just want to turn around and run away! So, let’s demystify it once and for all. The cytochome P450 (CYP45) system is basically the liver’s enzyme system. The CYP450 is so called because it is found within the membranes of a cell (hence CYTO). It contains a haem pigment (hence CHROME and P). And it absorbs light at a wavelength of 450nm. It has quite a number if functions…
- It is essential for the production of lots of things in the body including our cholesterol and natural steroids.
- It also helps detoxify the body of foreign chemicals
- It helps with the metabolisation of drugs (so they don’t linger about too long)
LIFESTYLE
BMI
Aim for healthy BMI <25 – consider dietition, Orlistat, other dietary measures & EXERCISE
ALCOHOL
Not to exceed recommended limits. (14 units men and women)
SMOKING
Stop!
BLOOD PRESSURE
Active management is essential!
Over half of all diabetics are hypertensive. Trials have shown that excellent BP control reduces retinopathy, nephropathy, strokes, heart failure and MI. BP control is as important as glycaemic control! TARGET < 130/80
Treatment
- 1st line – ACEi, ARB if they cannot tolerate it.
Ramipril starting regime derived from the HOPE study regime and BNF guidelines
If U&Es pre treatment reveal a creatinine < 150 micromol/l and a sodium >130 mmol/l then 2.5 mg Ramipril daily (1.25mg if on lower dose concomitant diuretics) for one week with check U&Es and an increase to 5.0 mg Ramipril for a further two weeks. Re-check U&Es and if indicated increase to 10mg Ramipril and repeat U&Es at least on an annual basis. If eGFR falls > 25% or creatinine rises by > 30% stop or back titrate treatment – see NICE guidelines. Don’t forget BNF cautions and contraindications. - 2nd line – CCB or, thiazide like diuretic or, Beta blocker (especially if there is a history of ischaemic heart disease),. Follow hypertension protocol
LIPIDS AND CVD RISK (see lipid modification protocol)
Offer generic Atorvastatin 40mg (Bradford Healthy Hearts) if their Q risk >10% (aged between 18-84 yrs), have been diabetic for > 10 years or, over 40 years old. Target chol <4mmol/l
For diabetics with established CVD offer secondary prevention or Chol > 4mmol/l – Atorvastatin 80mg
Triglycerides:
If TG level remains high (above 4.5mmol/l) please ref to CKS guidance on lipid modification or in-house lipid modification protocol.
Do not routinely offer Nicotinic acid or Omega fish oils.
MICROALBUMINURIA AND CKD
- All diabetics need testing annually for microalbuminuria and eGFR – microalbuminuria is the first sign of diabetic kidney disease and occurs before eGFR falls.
- SEE CKD PROTOCOL
ANTIPLATELETS
- Do not offer anti-platelets unless there is evidence of CVD
Why is the cytochrome P450 important?
Because so many drugs (including nutrients and herbal therapies) are metabolised via the CYP450 system. This system can be inhibited or induced by drugs. And that then leads to drug-drug interactions and all sorts of adverse reactions. Drugs that cause CYP450 drug interactions are referred to as either inhibitors or inducers.
- Inducers can increase the rate of another drug’s metabolism by x2/x3 fold over the period of a week! So, when an inducing agent is prescribed with another drug, the dosage of that other drug may need to be increased. Otherwise, the HIGHER rate of metabolism means the medication doesn’t last long and its therapeutic effect is reduced leading to therapeutic failure of that medication.
- Inhibitors can decrease the rate of another drug’s metabolism by x2/x3 fold over the period of a week! So, when an inhibitor agent is prescribed with another drug, the dosage of that other drug may need to be reduced. Otherwise, the LOWER rate of metabolism means the medication last longer and its therapeutic effect is enhanced leading to harmful adverse effects.
And what makes it worse, is that there is genetic variability in about 7% of people. For example, many clinicians believe that post menopausal women recieving tamoxifen for early breast cancer should be tested for their type of CYP2D6 genotype as it may be valuable in selecting the type of adjuvant homonal therapy to offer. And of course CYP2D6 inhibitors should be avoided in tamoxifen-treated women.
And patients come to us with often co-morbidity. It would be nice if the world was just full of people with just the one thing. But it isn’t. It’s a lot more complex. It’s not uncommon for a patient withy hypertension and bad lipids to present to us at some point with depression, for instance. Did you know that several antidepressants are CYP450 inhibitors (i.e. reduce metabolism of other drugs). The effect on drugs like halperidol or metoprolol will then be accentuated.
In the case of grapefruit juice, there are numerous medications known to interact with grapefruit juice including statins, antiarrhythmic agents, immunosuppressive agents, and calcium channel blockers. Furthermore, the inhibition of the enzyme system seems to be dose dependent; thus, the more a patient drinks, the more the inhibition that occurs. Additionally, the effects can last for several days if grapefruit juice is consumed on a regular basis. Luckily, the effect of this is not seen with other citrus juices.
Examples of INDUCERS
(i.e. speeds up metabolism of other drug, so it may not be as effective)
Mnemonic: SCRAP GPS
- Sulphonylureas
- Carbamezapine
- Rifampin
- Alcohol
- Phenytoin
- Griseofulvin
- Phenobarbital
- St Johns Wort
Examples of INHIBITORS
(i.e. slows down the metabolism of other drug, so it’s effects may be accentuated)
Mnemonic SICKFACES.COM G
- Sodium valproate
- Isoniazid
- Cimetidine
- Ketoconazole
- Fluconazole
- Alcohol..binge drinking
- Chloramphenicol
- Erythromycin
- Sulfonamides
- Ciprofloxacin
- Omeprazole
- Metronidazole
- Grapefruit Juice
Examples of drugs which interact with cP450 inducers/inhibitors
- Warfarin
- COCP
- Corticosteroids
- Tricyclics
- Statins
- Theophylline
- Pethidine
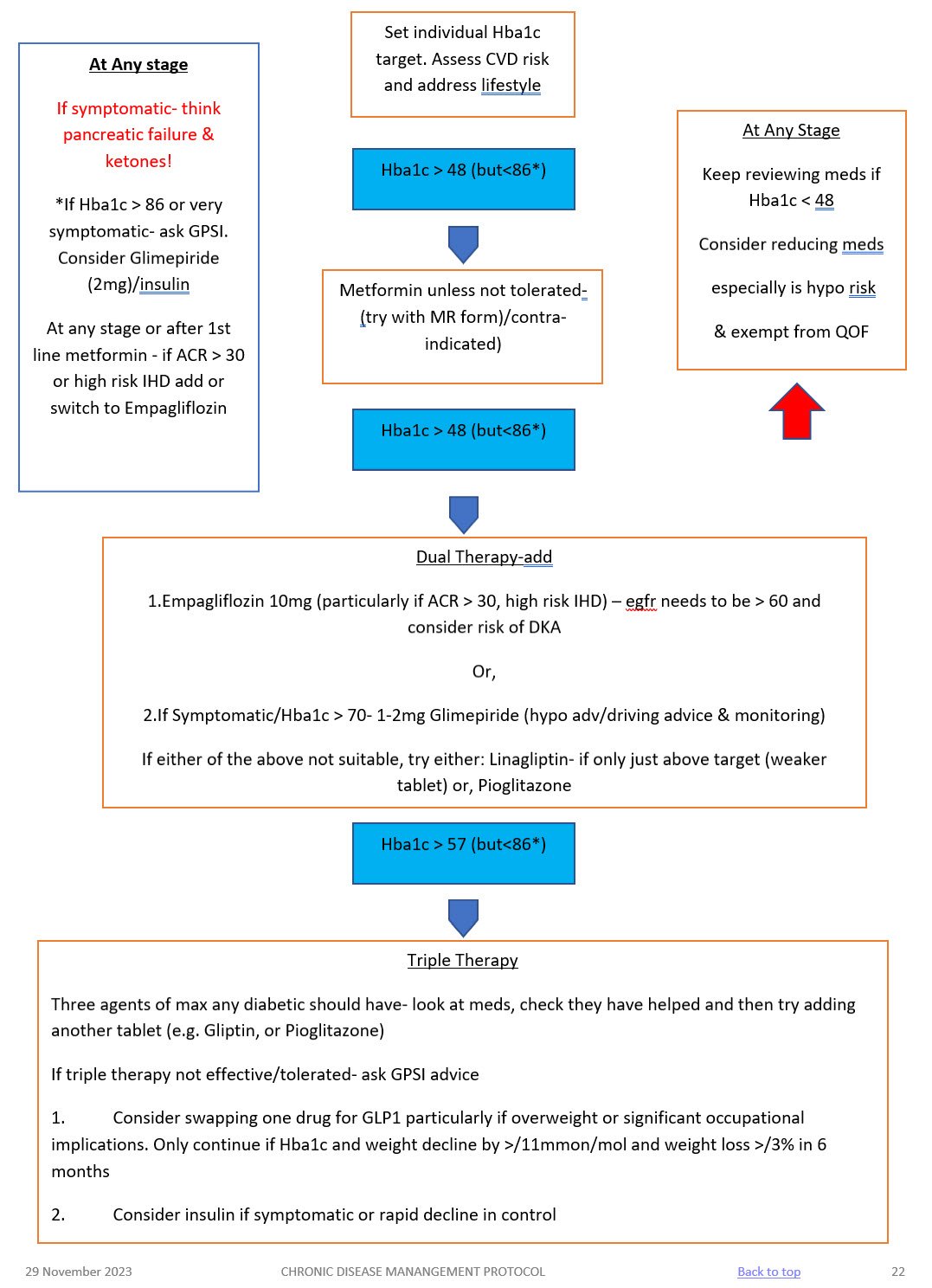
Medication | Mode of action | Side effects | Cautions (check BNF for more detail) | Dose |
METFORMIN 1st line treatment, unless BMI <25 (23 in South Asian population) Low Hypo risk Reduces CVD risk, weight neutral | Helps to stop the liver producing new glucose. It helps to overcome insulin resistance by making insulin carry glucose into muscle cells more effectively.
| Main side effect if GI affects, generally dose dependent-can be reduced with gradual increase in dose over several weeks or trying modified release Metformin Also: metallic taste, reduced absorption of vitamin B12, build up of lactic acid in the blood, allergic reaction and liver problems. | STOP/DO NOT USE IF eGFR <30 ml/min *Lactic acidosis- care if eGFR < 45ml/min. Document that advice has been given to stop these tablets if they become dehydrated (restart when eating normally again) *GI side effects. Titrate dose slowly to reduce side effects NOTE IF ALT> 3 TIMES NORMAL | Start at 500mg ideally with evening meal, increasing to 1g with evening meal after a week if they have no side effects. Max dose 2 gram over 4 weeks. Consider slow release for to reduce tablet load or if they are struggling with GI side effects.
|
SGLT-inhibitor Empagliflozin Low hypo risk Can help with weight loss | Sodium-glucose co-transporter 2 (SGLT2) inhibitor that prevents glucose reuptake in the kidney, leading to the excretion of excess glucose in the urine. | Polyuria, polydipsia, thrush. UTI, fluid depletion Increased risk of amputation- avoid if h/o leg ulcers | Only start if Cr Clearance > 60. Care if > 75 years. Risk of postural hypotension. Care needed if they have skin ulcers – risk of amputation. Document advice about normoglycaemic ketoacidosis and give ketostix. | Empagliflozin 10mg. Can be increased to 25mg. Expensive so only continue if there is a clear response after 6 months |
SULPHONYLUREA (SU) Glimepiride Risk of hypos Good if rapid response is needed. | They work by stimulating cells in the pancreas to make more insulin. They also help insulin to work more effectively in the body.
| Weight gain. Hypoglycaemia, gastrointestinal side effects, low sodium, facial flushing and intolerance of alcohol, allergies etc.
| Can cause hypoglycaemia, particularly if there is renal impairment or they are elderly. Consider occupation – hypos if not eating regularly, fasting. Make sure you give and document advice about hypos. Make sure they are able to test their blood glucose – issue glucometer, test strips, lancets and sharps bin. (SGBM) Document advice about driving/insurance. | Start at 1mg and titrate up to 4mg depending on glucose level. Should have an effect on Hba1c over a 2 month period. |
GLIPTIN Do not cause weight gain and encourages patient satiety. Although they probably reduce Hba1c levels less than other drug treatments. Low hypo risk | They work by blocking the action of the enzyme, DPP-4, which destroys the hormone Incretin.
| Gastro-intestinal effects, oedema, headache, Avoid if h/o Pancreatitis or heart failure or liver problems. | *Expensive- only continue if they meet NICE guidance. *Not v powerful max likely reduction ~ 11 mmol/mol *Do not use if a h/o pancreatitis *Monitor egfr at reviews *Don’t use if heart failure risk | Linagliptin 5mg if eGFR < 50 |
GLITAZONE Pioglitazone Low hypo risk Consider in people with very significant features of metabolic syndrome. South Asian | Reducing insulin resistance. Improving insulin sensitivity.
| Oedema esp if heart failure or at risk. Rare reports of liver dysfunction. Weight gain, gastro-intestinal side effects, headache, dizziness.
| Discuss with member of Level 2 team before starting. Avoid if they have heart failure or risk of fluid overload Avoid if h/o bladder cancer, undiagnosed haematuria Avoid if fracture risk Monitor LFTs at each diabetic review. Annual urine dip looking for haematuria | Pioglitazone:15mg-30mg. A six month period may be needed to really see an effect from these tablets. NICE recommends that they are only continued if at least a 11 mmol/l reduction in Hba1c is seen within 6 months of starting the treatment.
|
GLP-1 mimetic/insulin | Discuss with Level 2 doctor |
|
- At first warning of episode of hypoglycaemia:
- Immediately treat with a 15-20g of a short-acting carbohydrate such as:
- 200 mls of Lucozade (please note Lucozade formula has changed so lower in sugar- need 200ml)
- 200mls of non-diet drink
- 4-5 glucose tablets
- 3-4 jelly babies
- 200mls of fruit juice
- Immediately treat with a 15-20g of a short-acting carbohydrate such as:
- If the hypo is more severe, and the patient cannot treat themselves:
- applying Glucagel (or treacle, jam or honey) on the inside of cheeks and gently massaging the outside of cheeks.
- if unconscious, Glucagon can be injected if the person treating has been trained to use it.
- Otherwise call an ambulance immediately
- Important:
- If unable to swallow or unconscious, do not give anything by mouth (including Glucagel, treacle, jam or honey). Make sure family and friends are aware of this. If unconscious, place patient in the recovery position (on side with head tilted back) so that tongue does not block throat.
- Follow-on treatment:
- To prevent blood glucose levels dropping again, follow sugary foods with 10-20g of a longer-acting carbohydrate such as:
- half a sandwich
- fruit
- a small bowl of cereal
- biscuits and milk
- the next meal if due
- Patients experiencing regular episodes of hypoglycaemia require prompt review by the diabetes team.
- Severe episodes of hypoglycaemia require urgent review by the diabetes team.
- To prevent blood glucose levels dropping again, follow sugary foods with 10-20g of a longer-acting carbohydrate such as:
Advise patients the following: if you do go down with a cold, flu or any other illness…
- The Basics
- Rest.
- Drink plenty of sugar-free fluids.
- Avoid too much caffeine as this could make you dehydrated.
- Take painkillers in the recommended doses as necessary.
- Contact your GP to see if treatment with antibiotics is necessary.
- If you are vomiting uncontrollably, contact your GP or diabetes clinic.
- Insulin or diabetes medications
- Keep taking your insulin or diabetes medications even if you are not eating. Stop metformin and blood pressure medication if you are dehydrated. CONSIDER AKI SICK DAY RULES – see hypertension protocol.
- Testing
- Test your blood or urine four or more times a day and night (ie at least eight times in a 24-hour period) and write the results down. If you are not well enough to do this, ask someone to do it for you.
- Ketoacidosis
- When diabetes is out of control as a result of severe sickness, it can lead to a condition called diabetic ketoacidosis or diabetic coma if you have Type 1 diabetes. The body produces high levels of ketone bodies causing too much acidity in the blood.
- Testing for ketones
- If you have Type 1 diabetes and your blood glucose level is 15 mmol/l or more or you have two per cent or more glucose in your urine, you will also need to test your urine or blood for ketones. They are a sign that your diabetes is seriously out of control. Ketones are especially likely when you are vomiting and can very quickly make you feel even worse. If a ketone test is positive, contact your GP or diabetes care team immediately.
- Food and drink
- It is important to keep taking your medication as normal and drink plenty of sugar-free drinks. Aim to drink at least three litres (five pints) a day. Try to keep to your normal meal pattern, but if you are unable to, for any reason, you can replace some or all of your meals with snacks and/or drinks that contain carbohydrate such as yoghurt, milk and other milky drinks, fruit juice or sugary drinks such as Lucozade, ordinary cola or lemonade. You may find it useful to let fizzy drinks go flat to help keep them down
Advise patients of the following:
- Vaccinations and/or malaria tablets
- Carry diabetes ID or a GP letter if carrying insulin and list of prescription drugs
- Carry all medication and blood glucose testing equipment in hand luggage
- Consider how to keep insulin cool if travelling for long periods
- Travel insurance: – Allow 2 weeks to buy travel insurance. – Don‟t just buy on price, check the cover and read the small print – – Be honest and declare all medical conditions
- Plan to take twice the quantity of medical supplies normally used
- Consider adjusting medication if travelling across time zones
- Consider adjustment to insulin if travelling to hot or cold climate
- Carry a European Health Insurance Card (EHIC) if travelling within Europe
www.ehic.org.uk, / 0845 605 0707
Consider availability of insulin if travelling abroad for long periods.
Interpreting blood results on pathology template – Remember frailty
- HbA1c <48 →select satisfactory→take no action – patient will be reviewed as per recall
- HbA1c 48-53 →select abnormal →speak to nurse → send task to admin to book tel appt with nurse to discuss abnormal result and document a suggested plan to up-titrate medication based on the above guidance for nurse to discuss with patient – nurse will discuss with patient possible changes to medication and then task Dr back to make changes and issue script. – if on single drug or diet only
- HbA1c <53 → select satisfactory →take no action – if on SU or combination drugs patient will attend at next review 6 months later
- HbA1c >53 → select abnormal (take into account patients age and fraility) →speak to nurse → send task to admin to book tel appt with nurse to discuss abnormal result and document a suggested plan to up-titrate medication based on the above guidance for nurse to discuss with patient – nurse will discuss with patient possible changes to medication and then task Dr back to make changes and issue script.
Any concerns – send message to Level 2 team
Using the SystmOne Template (CDM) for Diabetes.
See CDM review table
- Bloods: U&Es, eGFR, HbA1c, ALT (if first year on statin) and lipid profile – (Consider other tests if have other chronic diseases.)
- Urine ACR.
- BP
- Lifestyle discussion: smoking status/cessation advice, exercise status, alcohol intake, diet.
- BMI
- Retinal review.
- Foot check annually (in house) and record on the template. If moderate or high risk they need a referral to podiatry
- Any complications? erectile dysfunction, neuropathic pain, autonomic neuropathy.
- Hypo unawareness, ? hypos requiring external intervention (see DVLA guidelines).
- Review of blood monitoring – if they require monitoring.
- Medication review: concordance/indications/side effects/if on insulin – injection sites.
- Record medication review done, move date on till next review
- Assign diagnosis to repeat template medication.
- Add/move recall on. NB: Diabetics well be reviewed at least 6 monthly.
TARGETS AT A GLANCE
- BP: <130/80 – particularly if there are renal problems
- Get to non smoking: don’t forget smoking cessation
- Cholesterol: < 4.0mmol/l
- HbA1c:
- Diet alone or single drug not affected by hypoglycaemia <48mmol/l
- Medication <53mmol/l. Patient tailored care needed especially if they are elderly or there are concerns about hypogylcaemia.
- BMI: <25
Diabetes in pregnancy is associated with risks to the woman and the developing fetus.
Planning a pregnancy
Women planning a pregnancy should be referred to a diabetes pre-conception clinic.
Pre-pregnancy planning includes:
- Diet and exercise, weight loss advised if body mass index > 27kg/m2
- Retinal photography unless carried out in last 12months
- Renal assessment (including microalbuminuria)
- Folic acid 5mgs for 3 months preconception and continued for first trimester.
- Establish rubella status, booster organised if required.
- Blood pressure should be monitored
- Smoking/alcohol cessation advice
Review of medications
- Metformin may be used before and during pregnancy, as well as or instead of insulin. The diabetes antenatal clinic will oversee their care whilst pregnant.
- Isophane insulin is the first-choice long-acting insulin during pregnancy.
- Discontinue oral hypoglycaemic agents (apart from metformin), ACE-inhibitors, Angiotensin Receptor Blockers and statins
Gestational diabetes
- 6 weeks post-partum patients require a HbA1c to establish whether glucose tolerance has returned to normal.
- All patients require advice on their elevated long term risk of diabetes.
- All patients require advice on their risk of gestational diabetes in future pregnancies.
- All patients require advice regarding diet, weight control and exercise
All patients require an ANNUAL HbA1c in view of their elevated risk of Type 2 diabetes. Please add an ‘AT RISK OF DIABETES’ recall to their notes.
Prescribing Theory - incl. cytochome P40 & prolonged QT interval
What is it?
When we mention the cytochrome P450 system, most doctors just want to turn around and run away! So, let’s demystify it once and for all. The cytochome P450 (CYP45) system is basically the liver’s enzyme system. The CYP450 is so called because it is found within the membranes of a cell (hence CYTO). It contains a haem pigment (hence CHROME and P). And it absorbs light at a wavelength of 450nm. It has quite a number if functions…
- It is essential for the production of lots of things in the body including our cholesterol and natural steroids.
- It also helps detoxify the body of foreign chemicals
- It helps with the metabolisation of drugs (so they don’t linger about too long)
Why is the cytochrome P450 important?
Because so many drugs (including nutrients and herbal therapies) are metabolised via the CYP450 system. This system can be inhibited or induced by drugs. And that then leads to drug-drug interactions and all sorts of adverse reactions. Drugs that cause CYP450 drug interactions are referred to as either inhibitors or inducers.
- Inducers can increase the rate of another drug’s metabolism by x2/x3 fold over the period of a week! So, when an inducing agent is prescribed with another drug, the dosage of that other drug may need to be increased. Otherwise, the HIGHER rate of metabolism means the medication doesn’t last long and its therapeutic effect is reduced leading to therapeutic failure of that medication.
- Inhibitors can decrease the rate of another drug’s metabolism by x2/x3 fold over the period of a week! So, when an inhibitor agent is prescribed with another drug, the dosage of that other drug may need to be reduced. Otherwise, the LOWER rate of metabolism means the medication last longer and its therapeutic effect is enhanced leading to harmful adverse effects.
And what makes it worse, is that there is genetic variability in about 7% of people. For example, many clinicians believe that post menopausal women recieving tamoxifen for early breast cancer should be tested for their type of CYP2D6 genotype as it may be valuable in selecting the type of adjuvant homonal therapy to offer. And of course CYP2D6 inhibitors should be avoided in tamoxifen-treated women.
And patients come to us with often co-morbidity. It would be nice if the world was just full of people with just the one thing. But it isn’t. It’s a lot more complex. It’s not uncommon for a patient withy hypertension and bad lipids to present to us at some point with depression, for instance. Did you know that several antidepressants are CYP450 inhibitors (i.e. reduce metabolism of other drugs). The effect on drugs like halperidol or metoprolol will then be accentuated.
In the case of grapefruit juice, there are numerous medications known to interact with grapefruit juice including statins, antiarrhythmic agents, immunosuppressive agents, and calcium channel blockers. Furthermore, the inhibition of the enzyme system seems to be dose dependent; thus, the more a patient drinks, the more the inhibition that occurs. Additionally, the effects can last for several days if grapefruit juice is consumed on a regular basis. Luckily, the effect of this is not seen with other citrus juices.
Examples of INDUCERS
(i.e. speeds up metabolism of other drug, so it may not be as effective)
Mnemonic: SCRAP GPS
- Sulphonylureas
- Carbamezapine
- Rifampin
- Alcohol
- Phenytoin
- Griseofulvin
- Phenobarbital
- St Johns Wort
Examples of INHIBITORS
(i.e. slows down the metabolism of other drug, so it’s effects may be accentuated)
Mnemonic SICKFACES.COM G
- Sodium valproate
- Isoniazid
- Cimetidine
- Ketoconazole
- Fluconazole
- Alcohol..binge drinking
- Chloramphenicol
- Erythromycin
- Sulfonamides
- Ciprofloxacin
- Omeprazole
- Metronidazole
- Grapefruit Juice
Examples of drugs which interact with cP450 inducers/inhibitors
- Warfarin
- COCP
- Corticosteroids
- Tricyclics
- Statins
- Theophylline
- Pethidine
Whst is the QT interval?
The QT interval is the measure of time between the onset of the Q wave and the end of the T wave. This interval represents the time that depolarization and repolarization of the ventricle occur.
Why is this important?
To understand why this is important, we need to talk for just a moment about the refractory period. After the cardiac cells depolarize, they must “recharge” or repolarize. This “recharging” phase is what we refer to as the refractory period. Generally speaking, a refractory period is one in which the cell is unable to have another action potential. More specifically, there’s an “absolute refractory period” where no new action potentials can take place…which is followed by a “relative refractory period” where an action potential COULD occur, if the stars are aligned, Venus is in Scorpio and everything falls into perfect place. But here’s the thing…you don’t want an action potential to occur during this time. If an electrical stimulus hits during this relative refractory period, premature depolarization can occur before the cardiac cells are completely repolarized…the result is that the heart can go into dangerous and deadly ventricular arrhythmias and ain’t nobody got time for that!
And this, ladies and gentlemen, is why we keep such a close eye on the QT interval.

Below is Torsades de Pointes

Definitions
Definitions for QT prolongation vary in the literature, but commonly the following are used
- but for men QTc >440 msec
- for women QTc >470 msec
When should I worry?
- QT interval varies dependent on the length of the cardiac cycle and is usually corrected (QTc) for heart rate.
- Correction of QT interval for heart rate is controversial and inexact. The reliability of the standard QTc decreases at higher heart rates.
- Several formulas can be used for this, most commonly Bazett’s formula is used (QTc=QT/√RR; QT interval in seconds, RR cardiac cycle in seconds)
- The other correction formulae are Frederica, Hodges or Framingham may be used.
- The major limitation of Bazett’s formula is that it overestimates QTc interval at any heart rate much higher than 60 beats per minute (bpm) and underestimates QTc interval at rates lower than 60 bpm.
- It is therefore recommended to use the Frederica formula if heart rate < 60bpm or >100bpm.
- The risk of TdP (Torsade de Pointes) increases with increasing QTc, for every 10 msec increase, there is a ~5-7% increase in the risk of arrhythmic events
- TdP = a form of tachycardia in which the electrical pulse in the heart undergoes a cyclical variation in strength, giving a characteristic electrocardiogram resembling a twisted fringe of spikes.
Below is Torsades de Pointes

So… look at the ECG!
Correct the QT interval using the fomula at MDCALC
Determine the increase from baseline
- MILD EFFECT: if the prolongation INCREASE is 10 msec or less, the effect is low and you don’t need to worry too much. However, be careful of co-prescribing several medications which are known to have a low effect because the combination might push the prolongation into the moderate or severe ranges!
- MODERATE EFFECT: if the prolongation INCREASE is 10-20 msec. This is clinically significant. Assess risk vs benefit. Consider dose reduction or switch to alternative. Monitor with repeat ECGs.
- HIGH EFFECT: if the prolongation INCREASE is greater than 20 msec, this is dangerous. You need to do something about it now! Assess risk vs benefit. Stop the offending drugs if possible or switch to alternative. Monitor with repeat ECGs.
Please note, this is NOT a comprehensive list. This is a list of common drugs seen in Primary Care/General Practice. You can see from the list below that a lot of drugs used in psychiatry do this.
MODERATE EFFECT
By moderate effect we mean an 10-20 msec increase in QT prolongation, which is significant. If the delay is greater than 20 msec, the risk is significant and serious!
Antibiotics | Erythromycin | Clarithromycin | Azithromycin | Ciprofloxacin |
Antidepressants | Citalopram | Escitalopram | Clomipramine | Quetiapine |
Anti-emetics | Ondansetron |
|
| |
Antifungals
| Fluconazole |
|
|
|
Anti-pychotics | Haloperidol | Chlorpromazine | Risperidone | Amisulpiride, |
Addiction Rx | Methadone (esp dose > 100mg) | Lofexidine |
|
|
Cardiac drugs | Amiodarone | Sotalol | Flecainide |
|
Miscellaneous | Hydroxyzine (anti-itch) | Hydroxychloroquine (anti-malarial) | Tolterodine (urology) | Quinine (e.g cramps) |
| Sildenafil |
|
|
|
MILD/LOW EFFECT
The following drugs can also cause a QT prolongation but the effect is usually MILD or LOW. (i.e. less than 10 msec). Usually you don’t need to worry. However, the effect can be greater and therefore more serious if you use a combination of the mildly prolonging QT interval drugs. So be careful with co-prescribing these drugs in the same patient.
- Psychiatry drugs – Amitriptyline, Fluoxetine, Mirtazepine, Trazadone, Venlafaxine, Lithium (mood stabiliser), Resperidone, Olanzapine, Clozapine, Aripiprazole, Buproprion, Duloxetine, Memantine (dementia)
- Pain relief – Buprenorphine
- Anti-emetics – prochlorperazine
Lots of things can cause a prolonged QTc…here are just a few:
- ischemic cardiac tissue or s/p cardiac arrest
- electrolyte imbalances (K, Mg, Ca)
- hypothermia
- increased ICP
- congenital long QT syndrome (an inherited faulty gene disorder) – often asymptomatic, others get blackouts, palpitations, seizures before age 40. Leading cause of sudden death in young people. Thank goodness it is uncommon though – 1 in 2000.
Practical Prescribing & Medication Reviews
General Principles…
- Keep to generic prescribing (Except if brands are cheaper, prescribe inhalers as brand)
- Avoid combined products – obviously, in some conditions you have to.
- Avoid sleeping tablets for sleep problems
- Avoid orodispersible as more expensive
- Avoid liquid medicines for adults – v. expensive
- Avoid initiating dietary supplements – refer to malnutrition pathway (ASSIST) and then dietician, if needed consider Complan/Aymes
- Avoid ‘Specials’
- No Glucosamine
- OTC items – limit prescribing – Patient to buy if possible
- Consider prescribing Vs Non prescription, e.g lifestyle. Don’t prescribe a pill for every ill! e.g sore throat – is difflam really necessary in every case? Nasal saline drops for a congested nose – does it really help? Haven’t we survived hundreds of years without it? Is it life changing?
- Issue medication electronically where possible. You are more likely to make a mistake with handwritten notes. Even on a home visit, consider telling the patient that you will issue the medication electronically to their pharmacist and what time to go and pick it up.
Writing a prescription…
- Never use ASD (as directed) as an instruction on a prescription. Spell out the dose precisely. How is the patient meant to know if you don’t spell it out?
- Complicated liquid medicine doses – let the pharmacist work out the mls. You just write out the prescribed dose in mg. For example, if there is a drug called Nuisancia and you want to give 15mg bd and it comes 20mls/5ml, just write Nusiancia (20mg/5ml) 15mg bd. The pharmacist will work out the dose in mls (which in this case would be 3.75mls bd). They will work out the mls and instruct the patient and will give them a syringe and show them what to do. It is, after all, part of their specialty skills.
- Usually can give up to 2 months supply at a time
- 3m repeats if going out of the country (or job involves being away for long periods of time e.g. cruise ship workers, oil rig works etc)
- Consider a much less frequency if high risk drug or control drugs
- If any special monitoring required – add as reminder on home screen AND the script notes. Add recall date.
- If adding medication started by hospital, add date of letter to script notes
The following will save NHS costs…
- Sukkarto should be generic
- No bath emollients or shower gels- just use normal emollient
- No branded erectile dysfunction Rx- the generics are pennies now
- No-one should be on liothyronine, apart from a very few patients where it will be initiated by secondary care
- No unlicensed melatonin
- No unlicensed colecalciferol– they can be thousands of pounds when we can prescribe the same for a few quid
- Only low cost pen needles and blood glucose testing strips
- Be careful of prescribing liquids and suspensions esp in adults. For example Nitrofurantoin tablets are pence. But Nitrofurantoin suspension is like £500! General rule of thumb: if they are eating food, then can take tablets.
- Reduce prescription request burden for regular medications
- Ensure disease control targets are being optimised to patient tolerance
- Aim to have patients annual reviews for all CDM (Chronic Disease Medication) together
- To set dates correctly to enhance patient safety: medication review dates on repeat template should match or be a few beyond the recall dates wherever possible
Place drug onto repeat template if:
- Medication for chronic disease
- On hospital discharge for long term use
- Review of hospital/specialist letter amend repeat medication as required
- Emollients if regularly used
- Pain relief/anti-depressants/anti-psychotics – see below
- BE SAFE AND USE COMMON SENSE – if unsure – ASK!! – BHMP clinical meeting task group
And remember…
- Remove un-used/unnecessary items from repeat template
- Restrict for clinician issue only if high risk/monitoring needed, as in don’t want admin to issue from repeat template
- Dosette scripts to be done as 28 days
- i.e 7 x 4 trays to be given to patient in one go
- if weekly issues are specifically needed then set quantity to 7 day issues
- add in script notes *** Dosette Tray *** if needing to be added to tray
This is what you need to do when you receive a script request from the patient, the first thing to do is CHECK THE MEDICATION REVIEW DATE
- if within review date
- issue the medication
- if review overdue
- book patient in for medication review
- advise them that they will have difficulty receiving the medications until review has been done.
- if patient says they have completely ran out of medication – then send a prescription request to the difficult script task group and book it onto the daily pharmacy ledger.
- Identify which chronic diseases are being reviewed
- Review appropriate clinical protocol/template
- Review patients well being
- Review understanding of disease condition and how they are coping
- Discuss lifestyle measures
- Undertake necessary monitoring requirements: e.g annual pathology, ECG, spirometry, foot checks etc
- Discuss medication and identify any problems
- TASK the “CHRONIC DISEASE” user group under “CHRONIC DISEASE MEDICATION REVIEW” task or the prescribing team
TASKS
- Quick scan of new journal to see if any outstanding requirements – Look at outstanding QoF targets/other alerts (can be seen on home page)
- Review nurse entry, identify any problems
- Review once all pathology results are back. Aim to complete within 3-4 days of receiving the task
- Review CDM table to ensure all monitoring has been done
- Review BP aim for target as per protocol
How to review medication
- For all CDM meds that have been reviewed by nurse review, move dates on to match/or a few weeks beyond recall date (could be moved on by the nurses if trained), if all parameters are satisfactory.
- For other meds or med problems that have been identified by the nurses.
- Check if a review has been done recently.
- If no review done – task admin/SMS patient to book review.
- If problems related to meds highlight then task to pharmacist to do med review.
- If meds have been reviewed in the previous year by Dr/nurse/ pharmacist and if no problems identified then just move date on to tally with CDM recall if it’s clinically safe.
- Check if a review has been done recently.
Review pathology results as required:
- U+Es – worry if the trend is falling! (done for a lot of chronic disease reviews)
- Hba1c (targets for DMs and recognise at risk groups)
- LFTs (drug monitoring e.g NOACS, antipsychotics, Amber and high risk drugs)
- FBC (drug monitoring e.g NOACS, antipsychotics, Amber and high risk drugs)
- Lipids (Qrisk ? statin start or increase)
- Urine acr
- IF PATIENT ELIGIBLE FOR SMR (see the clinical system HOME page) :
- If straight forward – no changes required/good concordance/no polypharmacy/no frailty issues – move the date on and tick the SMR box
- If complicated – then task pharmacist to book for a SMR review
KEY POINTS
- If review date is up and a pharmacist review is needed, just move date by 1-2 months so patient does not struggle to get their medications if it’s safe.
- Please be aware that some meds e.g Amber drugs, high risk drugs that need monitoring, antipsychotics, strong pain relief, antidepressants may not tally with the CDM review as they have their own planned monitoring.
- Most CDM meds will be moved on for 1 year, others for 6 months depending on the next recall dates.
- Review dates add an extra safety net for patients to ensure they are receiving the appropriate monitoring for the medication that they are using.
Prescriptions can be requested:
- During consultation – medication review
- By any Dr – patient encounter
- By nurses during their consultations
- via a Chronic disease medication review request
- Online account – by patient/carer
- E-consultation
- By telephone only if prior agreement is in place – e.g housebound patients
When reviewing repeat medications
- Max 2m supply – however 3m supply on NHS especially if going out of country. Control Drugs/high risk drugs at clinician discretion if appropriate
- Any special monitoring information place as a reminder on the home screen, add a Recall and date appropriately, add script notes when setting up repeat template for drug.
- If medication started in secondary care helpful to write the date of the communication in script note when adding to repeat template.
- Check for chronic disease monitoring – add relevant recall
- Check for outstanding QOF prompts. Remember Smears!!
- Check compliance/concordance/indications/interactions/dosage/side effects/quantity/cost
DEMENTIA
– Degree of cognitive impairment leading to sig. Memory problems, a degree of disorientation, or a change in personality & unable to self care
– MiniCog tool (easy to use assessment tool)
– HbA1c target: 60-70mmol/mol
END OF LIFE CARE
- Significant illness or malignancy & have life expectancy reduced to <1 year
- Glycaemic aim – hypo and symptomatic hyperglycaemia avoidance
Signing prescriptions:
- You will be asked to sign prescriptions regularly.
- Before you do, make sure the repeat list are all drugs that should be on repeat.
- If there are drugs that are meant to be given acute, but being asked repeatedly for by the patient – do not issue. Question, discuss and educate the patient.
- If there are drugs that need monitoring – check to see if those monitoring items have been done (like P, BP, ECG, bloods).
List of Drugs that need monitoring
ANTIPSYCHOTICS – like Amisulpride, Aripiprazole, Chlorpromazine, Clozapine, Flupentixol, Haloperidol, Olanzapine, Quetiapine, Risperidone, Sulpiride, Trifluoperazine, Zuclopenthixol
- NOACS – like Apixaban, Dabigatran, Rivaroxaban – fbc, u+es, lfts, annually
AMBER DRUGS – see list below
Don’t forget Amiodarone
|
Alcohol withdrawal |
|
|
Mild to moderate dementia in Alzheimer’s disease |
|
|
Dopaminergic drug – Parkinson’s disease |
|
|
Treatment of ADHD |
|
|
Immunosuppression |
|
|
Inflammatory Bowel Disease |
|
|
Immunosuppression in adults |
|
|
Renal |
|
|
Secondary hyperparathyroidism in end stage Renal disease |
|
|
Treatment of colonisation and infections of the lung due to pseudomonas aeruginosa |
|
|
Primary and secondary prevention of osteoporotic fractures in postmenopausal women |
|
|
Treatment of ADHD |
|
|
Phosphorylated glycosylated recombinant hyman deoxyribonuclease 1 (rhDNase) – Cystic Fibrosis |
|
|
Renal Anaemia |
|
|
Breast Cancer |
|
|
Treatment of grass pollen allergies |
|
|
TBC |
|
|
DMARD and immunosupression |
|
|
Metastatic bone disease |
|
|
Treatment of depressive illness |
|
|
Disease modifying anti-rheumatic drug |
|
|
Attention Deficity Hyperactivity Disorder |
|
|
Affective disorders and cluster headaches |
|
|
Sleep disorders |
|
|
Immunosuppression |
|
|
Treatment of ADHD |
|
|
For the management of Status Epilepticus in adults and children |
|
|
Narcolepsy |
|
|
Immunosuppression |
|
|
Mycophenolate Mofetil or Mycophenolic Acid (Myfortic) Post Solid Organ Transplant |
Post renal transplant |
|
Alcohol relapse prevention |
|
|
Treatment of narcotic addiction |
|
|
Disease-modifying anti-rheumatic drug – rheumatoid arthritis |
|
|
Treatment of depressive illness |
|
|
Chemoprevention of amilial breast cancer |
|
|
Treatment of amytrophic lateral sclerosis |
|
|
Immunosuppressant post renal transplant |
|
|
Sodium Aurothiomalate (Gold Injection) in Rheumatoid Arthritis |
Disease-modifying anti-rheumatic drug – rheumatoid arthritis |
|
Somatostatin Analogues (Somatuline LA, Somatuline Autogel and Sandostatin LAR) * |
Somatostatin Analogue – licensed indications (symptoms associated with carcinoid tumours with features of carcinoid syndrome, VIPomas, glucagonomas, acromegaly, prevention of complications following pancreatic surgery) |
|
DMARD and immunosupression |
|
|
Immunosuppression post transplant |
|
|
Chemoprevention of familial breast cancer |
|
|
Treatment of male hypogonadism menopausal symptoms in women |
|
|
Cystic fibrosis management |
|
|
Treatment of depressive illness |
|
|
Cluster headaches |
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Prescribing Pearls
- Try not to give “a pill for every ill” – promote self-help and less reliance on the doctor for small illnesses.
- Drugs which often interact with other drugs and to be cautious off when adding more medication…
- Gentamycin
- Warfarin
- Lithium
- Digoxin
- Theophylline
- Methotrexate
- Phenytoin
- Insulin
- Cyclosporin
Generally
Don’t forget – follow the WHO pain ladder, starting with Paracetamol if needs be, then co-codamol, co-dydramol, tramadol etc. Don’t just give randomly. If you ever get stuck with a patient’s pain control, go back to the WHO pain ladder.
NSAIDs: remember, Naproxen better than ibuprofen. Better safety profile, stronger. Needs to give PPI if over age 65 OR high risk factors. High risk factors: PMH of gastric/duodenal ulcers, GI bleeding, blood thinning agents, aspirin 300mg, prednisolone, SSRIs (yes, SSRIs can increase risk of GI bleeds). COX2 inhibitors better than ibuprofen and naproxen for GI risks.
NSAID gels: Would gels be safer than oral NSAID? Ibugel. Voltarol gel. Piroxicam gel Ketoprofen gel
COX2 inhibitors or high dose ibuprofen (<2400mg daily): do NOT prescribe if patient has IHD, PVD, CVD, CHF grade 2-3. Also don’t give COX2 inhibitors to those with Inflammatory Bowel Disease.
Other Non-opioids: think amitriptyline, gabapentin (generally try and avoid pentins if you can)
More about the COX-2 inhibitors
NSAIDs reduce the production of prostaglandins by inhibiting the enzyme cyclo-oxygenase. They vary in their selectivity for inhibiting different types of cyclo-oxygenase (COX1 and COX2). Naproxen and Ibuprofen inhibit both COX1 and COX2. COX2 inhibitors like etoricoxib and celecoxib, inhibit only cyclo-oxygenase-2 (COX-2) – which is associated with less gastro-intestinal intolerance.
- The selective inhibitors of COX-2, etoricoxib and celecoxib, are as effective as pain killers as non-selective NSAIDs such as naproxen and ibuprofen.
- Celecoxib and etoricoxib are licensed for the relief of pain in osteoarthritis, rheumatoid arthritis, and ankylosing spondylitis; etoricoxib is also licensed for the relief of pain from acute gout.
- Although selective inhibitors can cause serious gastro-intestinal events, available evidence appears to indicate that the risk of serious upper gastro-intestinal events is lower with selective inhibitors compared to non-selective NSAIDs
- But this advantage may be lost in patients who require concomitant low-dose aspirin.
A rundown of the NSAIDs
- Ibuprofen: It has fewer side-effects than other non-selective NSAIDs but its anti-inflammatory properties are weaker. It is unsuitable for conditions where inflammation is prominent. Dexibuprofen is the active enantiomer of ibuprofen. It has similar properties to ibuprofen and is licensed for the relief of mild to moderate pain and inflammation.
- Naproxen: is one of the first choices because it combines good efficacy with a low incidence of side-effects (but more than ibuprofen).
- Ketoprofen: has anti-inflammatory properties similar to ibuprofen and BUT has more side-effects. Dexketoprofen, an isomer of ketoprofen, has been introduced for the short-term relief of mild to moderate pain.
- Etodolac: is comparable in efficacy to naproxen; it is licensed for symptomatic relief of osteoarthritis and rheumatoid arthritis.
- Indometacin: has an action equal to or superior to that of naproxen, but with a high incidence of side-effects including headache, dizziness, and gastro-intestinal disturbances.
- Mefenamic acid: has minor anti-inflammatory properties. Occasionally associated with diarrhoea and haemolytic anaemia which require discontinuation of treatment.
- Meloxicam: is licensed for the short-term relief of pain in osteoarthritis and for long-term treatment of rheumatoid arthritis and ankylosing spondylitis.
- Nabumetone: is comparable in effect to naproxen.
- Piroxicam: is as effective as naproxen and has a long duration of action which permits once-daily administration. However, it has more gastro-intestinal side-effects than most other NSAIDs, and is associated with more frequent serious skin reactions.
- Tolfenamic acid: is licensed for the treatment of migraine.
- ACE inhibitors – don’t forget to tell patients they need a U&E 2 weeks after starting to check their kidneys handle it okay.
- Do not prescribe Verapamil with Diltiazem (mnemonic VD).
- Reduce diuretics in the elderly during Summer time (otherwise can dehydrate).
- Know the features of Digoxin toxicity (and monitor blood levels).
- For palliative heart failure:
- Disease-modifying therapies at maximally tolerated doses also help to alleviate symptoms. This includes ACE inhibitors, beta-blockers and aldosterone antagonists.
- Opioids can be useful for managing breathlessness in heart failure.
- Low dose oral morphine is the usual first line opioid (e.g. morphine MR 5mg BD or 2.5-5mg morphine PRN).
- If there is significant renal impairment (eGFR <50) then consider low dose PRN morphine or oxycodone first line instead – discuss with specialist palliative care if unsure.
- Evidence suggests that when used for breathlessness, opioid doses in excess of morphine 30mg (or equivalent) are associated with increased mortality, so total daily doses should remain below this
- Remember, steroid creams cause skin ageing with long term use. Don’t get me wrong – they are great for some skin problems like eczema but limit them to 2 weeks use. And tell all patients how they will ruin the skin if used continuously long term without thought.
- With steroids – try and use ointments rather than creams – better penetration.
Steroid Cream Strength
- Mild
- Hydrocortisone 1%
- Mild/moderate
- Eumovate
- Moderate
- Momentasone (Elocon)
- Beclomethasone valerate 0.025%
- Potent
- Dermovate
- Be careful when prescribing insulins – errors in prescribing can cause death. Double check the dose.
Be careful with prescribing a medicine which may cause dependence . As a doctor, don’t take the easy way out by providing a quick fix to chronic pain or difficulties by simply prescribing these sorts of drugs. Instead, discuss alternative ways of managing the pain or difficulty (coping mechanisms), optimise their lives (e.g. otherways to improve mood and happiness, mindfulness) and empower the patient. And whilst we say avoid their use generally across all age groups, especially avoid in those under age 65. Remember, starting a person even at the age 66 means they’re likely to be on them for 15 years (average life expectancy about 83) – and in that time, they will want more and more, year on year! These drugs in higher doses as more and more get pile on then start destroying the lives of these patients. The number of patients who say how amazing their lives are when they gradually withdraw from years of being hookeed is quite high. The top 4 culprits are
- Opioids (including tramadol)
- Gabapentinoids (like gabapentin and pregablin)
- Benzodiazepines (like diazepam, lorazepam and temazepam)
- Z-drugs (the sleeping tablets – like Zolpidem and Zopiclone)
- Thyroxine replacement – be guided by the TSH level generally when deciding whether to increase, decrease or maintain the levothyroxine dose.
- Try not to give nasal steroid sprays willy nilly. Remember, long term use will damage the nasal mucosal membrane causing even more difficult problems to treat in the future.
- Remember to de-prescribe if polypharmacy. Click here for more on de-prescribing and specific notes on specific drugs.
- There is good evidence that stopping psychotropic drugs (including opioid analgesics) can reduce falls. Taking a psychotropic medication approximately doubles the risk of falls.
- Nitrofurantoin: long-term (greater than six months) use of nitrofurantoin is associated with pulmonary toxicity. CARM have received over 60 reports of serious pulmonary reactions following the use of nitrofurantoin.
- Overactive bladder or incontinence medications: consider withdrawing if any dizziness, confusion, blurred vision or drowsiness.
- Nutritional supplements: Discontinue when prescribed for prophylaxis rather than treatment of malnutrition.
- Remember sick day rules & prescribing – click here
- Reduce diuretics in the elderly during Summertime (otherwise can dehydrate).
- Remember, Lansoprazole cover for those who will be on long term NSAIDs or >= age 65
- Also, patients often get left on Lansoprazole 30mg – step down to 15mg where possible.
Ferrous fumarate/sulphate or Folic acid – issue 3/4m course. That’s what is needed to get the stores back up. Don’t repeat bloods until 3m is up.
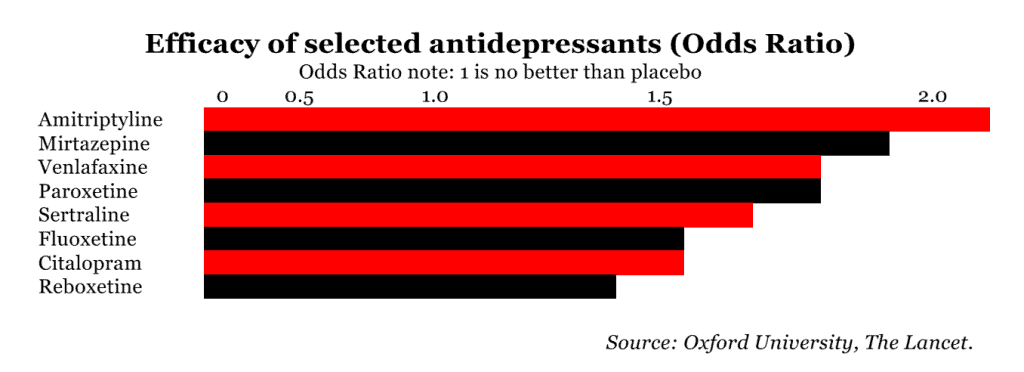
- Antidepressants take about 4-6 weeks to work. So tell patients to persevere for 4 weeks when starting or changing dose regimes.
- Do not over emphasise that some antidepressants can make you feel worse than better initially. If you over-egg this, then more patients are likely to experience this because of the nocebo effect (opposite of the placebo effect).
- If coming off SSRIs – do it slowly. Otherwise withdrawal effects.
- No Paroxetine/Fluoxetine for those on Tamoxifen – use Citalopram instead. Paroxetine and fluoxetine should not be prescribed for depression or hot flashes in women who have had breast cancer and are now taking tamoxifen to prevent a recurrence. Citalopram or venlafaxine should be considered instead. This message comes from a study showing that paroxetine, by interfering with the metabolism of tamoxifen, reduces or abolishes its protective effect against breast cancer recurrence, and that women taking both drugs have an increased risk for death from breast cancer. Paroxetine is a strong inhibitor of the CYP2D6 enzyme that converts tamoxifen to its active metabolite, reducing the amount of active drug that is released
- Do not prescribe B-Blockers in Asthma
- Know the features of Lithium toxicity & monitor blood levels.
Propranolol – remember, if your patient has a moderate to high suicidal risk, do not prescribe – high risk of death in suicidal attempts! Propranolol is used to treat several medical conditions, including migraine, cardiovascular problems, and the physical effects of anxiety. But there has been a rise in propranolol overdose deaths in the last few years (2020). If prescribing, tell patients about the possible severe consequences of overdose with propranolol and that it can cause death. Prescribers should be mindful of quantities supplied on a prescription, particularly where there is a significant risk of overdose. Where an opportunity arises, please consider reviewing the ongoing need for propranolol.
- Naproxen vs Ibuprofen vs Diclofenac – Don’t use diclofenac (high risk of GI ulcers and bleeds). Naproxen safer, even more so than Ibuprofen. May need to prescribe with PPI esp if age =>45 (see CKS guidance).
- Do not prescribe pentins in general (e.g. gabapentin, pregabalin)
- Do not generally prescribe diazepam for back pain.
- Capsaicin – remember, if using, only use a small amount to rub in. Too large a blob, and all that will result is chilli-like burning.
- Prescribing for children – think of their weight, and use a weight estimation formula if necessary.
- True Cow’s Milk Allergy vs
- weight in Kg = (age in years + 4) x 2
- 3 months = 6 Kg
- 6 months = 8 Kg
- 9 months = 9 Kg
HOW MUCH SHOULD BABIES BE FEEDING?
- Newborns & First few weeks: 1.5–3 ounces (45–90 milliliters) every 2–3 hours. Increases as baby grows.
- 2 months: 4–5 ounces (120–150 milliliters) every 3–4 hours.
- 4 months: 4–6 ounces (120-180 milliliters) at each feeding, depending on how often they eat.
- 6 months: 6–8 ounces (180–230 milliliters) about 4–5 times a day.
- Try not to give any pentin drugs like gabapentin (black market for selling).
- If you are using pentins, remember titrate up. When taking off, titrate down! Otherwise, can have fits!
- Try not to give benzos like diazepam, lorazepam (addiction problems highly likely)
- Try not to give Z drugs like zopiclone, zolpidem (dependency problems) – besides, regular use after 2 weeks >>> they STOP working!
- Eye ointment is better usually than eye drops for things like chloramphenicol. Sticks to the eyes rather than gets drained down the nasolacrimal duct.
- Try and avoid pentins if you can – e.g. gabapentin, pregablin.
- If patients are on anti-epileptics, double check interactions when prescribing. Anti-epileptics are notorious for drug interactions!
- Do not prescribe B-Blockers in Asthma
- Be careful with steroids – if longer than 2 weeks, taper down, do not stop suddenly. See below.
- If giving steroids (e.g. prednisolone) for more than 2 weeks, taper down! Do not stop suddenly. The risk of adrenal crisis is particularly high if 4 weeks duration.
- What makes me more likely to have adrenal insufficiency?
- Taking steroid medication can interfere with your adrenal glands from making cortisol and cause adrenal insufficiency.
- Your risk of this happening increases if you:
- are on oral steroids for 4 weeks or longer
- take repeated short-term courses of oral steroids
- take high-dose inhaled steroids
- have repeated steroid injections into your joints or muscles
- use steroids in any form and take certain drugs, such as some antivirals, some antifungals and an antibiotic called clarithromycin, if used long term
- are on multiple preparations of steroids.
- This risk lasts for up to 12 months after you stop regular steroid medication.
- If you have been on a long course of steroids, as described above, you must not stop taking this medication unless you have been advised to do so by your healthcare professional.
- What is adrenal insufficiency?
- Cortisol is your body’s natural steroid hormone. It plays many vital roles in maintaining and regulating normal healthy body functions, particularly when you are ill or under stress.
- Adrenal insufficiency is where your adrenal glands do not make enough cortisol.
- If you have adrenal insufficiency and do not get enough steroid medication, particularly when you are ill or having a procedure or surgery, you could become dangerously ill with adrenal crisis.
- What are the symptoms of adrenal insufficiency?
- Symptoms of long-term (chronic) adrenal insufficiency include: (Note that they are vague)
- feeling more tired
- feeling dizzy
- feeling sick
- loss of appetite
- weight loss.
- Symptoms of adrenal crisis (acute adrenal insufficiency), which means you need to see medical attention urgently includes:
- nausea and vomiting
- collapse
- low blood pressure
- confusion
- pale skin and sweating.
- Symptoms of long-term (chronic) adrenal insufficiency include: (Note that they are vague)
- What can I do to stay safe?
- Always carry your Steroid Emergency Card with you.
- This tells other people that you are currently or were recently on steroid medication.
- Ask for one from your community pharmacy, GP (home doctor) or hospital team, or download it from: https://pituitary.org.uk/media/615391/Steroid-card-v2-.pdf
- When prescribing morphine, or End Of Life medications, double check your calculations
- If a patient’s pain is not controlled, increase the 24h opioid dose by 1/3rd. So, if they are on MST 30mg bd, increase to 40mg bd.
- If you are increasing the regular pain relief dose, then remember to increase the breakthrough dose too.
- The breakthrough dose of opiates is 1/6th of the total daily dose of opiates.
(MST 15mg bd = breakthrough dose 5mg oramorph. MST 30mg bd = breakthrough dose = 10mg oramorph). Please double check with senior if unsure.
Remember to calculate this and include patches as well as oral medications and syringe drivers. Ask palliative care for advice if needed. - When starting a syringe driver don’t remove an existing opiate patch but continue to change it when scheduled.
If their background opiate analgesia needs to be increased add it into the syringe driver and update the PRN dose calculation. - Remember not all pain is opioid responsive.
It can be helpful to ask the patient whether previous background dose increases made a difference or whether PRN opioid doses help- if the answer is no, consider adding an adjuvant rather than continuing to increase opiates. For example, bone pain from bone mets – usually responds better to NSAIDs than opioids. - Know the features of opioid toxicity (confusions, picking at things in mid air, hallucinating). Most likely if opioid doses increased too much too suddenly.
- Always double check or even triple check your calculations. Ask a colleague to double check if you want to be even more safe.
- Levomepromazine is an excellent anti-emetic in palliative care which covers a wide range of receptors and has a long half-life.
The oral and sub-cutaneous dose for nausea is 2.5-6.25mg.. The 25mg tablets cut into quarters are considerably cheaper than the 6mg tablets but you may need to switch to these if the 6.25mg dose is too sedating. - There are loads of good guides on palliative care symptom control drugs (e.g. nausea, vomiting, constipation, pain and so on). See resources in Palliative Care section.
- For palliative heart failure:
- Disease-modifying therapies at maximally tolerated doses also help to alleviate symptoms. This includes ACE inhibitors, beta-blockers and aldosterone antagonists.
- Opioids can be useful for managing breathlessness in heart failure.
- Low dose oral morphine is the usual first line opioid (e.g. morphine MR 5mg BD or 2.5-5mg morphine PRN).
- If there is significant renal impairment (eGFR <50) then consider low dose PRN morphine or oxycodone first line instead – discuss with specialist palliative care if unsure.
- Evidence suggests that when used for breathlessness, opioid doses in excess of morphine 30mg (or equivalent) are associated with increased mortality, so total daily doses should remain below this
- XXXX
- XXXX
- If something ever gives you significant diarrhoea or vomiting (or both), it can affect your contraceptive pill’s effectivness. This include vomtiing/diarrhoea from a tummy bug or a side effect of a drug like antibiotics or the weightloss drug Orlistat. If this is the case, then use double protection – continue to take the pill and use another method like condoms for the duration of the vomiting/diarrhoea and 7 days after.
- Most common antibiotics (amoxicillin, penicillin, trimethoprim, erythromycin) do NOT affect the pill UNLESS you get bad diarrhoea or vomting with them. The only uncommon antibiotic that can affect the contraceptive pill are the antibiotics to treat TB – rifampicin and rifabutin.
- Enzyme inducing drugs can also reduce those on the COMBINED pill (i.e. enzyme inducers “process” the drug faster”). Enzyme inducers include: rifampicin (not a common antibiotic; used for TB), some antiepileptic meds, HIV meds, St Johns Wort.
The MRCGP Prescribing Assessment
Prescribing is an integral part of a General Practitioner’s work and several high profile cases have been published when qualified doctors have made catastrophic errors. Because there are a large number of patient deaths relating to medication errors. The only way this will improve is if we start regularly reviewing and analysing our prescribing habits. The best way of looking at an identified need is to pause and reflect on what we are doing rather than bury our heads and just continuing as we are. Would you agree?
We know GP trainees appear to assessed left-right-and centre. But this is another important area where we can better ourselves. Qualified GPs and their practices are often asked to look at their prescribing habits in some way or another and we feel therefore trainees should too.
All prescribing GPs are expected to demonstrate the following, across people of all ages which includes extremes of age, for example babies, children and older people with frailty (based on the GMC GPCs 2017). The items on the right are the proficiencies being assessed.
- Assesses the risks and benefits including those posed by other medications and medical conditions, reducing polypharmacy where possible.
- Identifies when prescribing unlicensed medicines and informs patients appropriately.
- Adheres to national or local guidelines (including recommendations for over the counter prescribing (OTC) and evidence-based medicine.
- Uses antimicrobials appropriately.
- Counsels patients appropriately including giving instructions for taking medicines safety in line with up to date literature.
- Reviews and monitors effects including blood testing at appropriate intervals.
All trainees in ST3 have to do one. There is no set standard as it is designed as a learning exercise; however if no errors are highlighted and if no learning is identified this would raise concerns, as to date this has never been the case.
- The trainee does a computer search on their last 50 retrospective prescriptions from a set date
- Using the prescribing manual, the trainee reviews these prescriptions & maps them against potential prescribing errors in the spreadsheet provided. Any issues are highlighted and investigated for possible causes and methods of avoidance suggested.
- The GP trainer/Supervisor reviews 20 of these prescriptions (including those where the trainee has NOT identified errors), and maps these against potential errors and adds these to the spreadsheet
- The trainee completes the trainee reflection form in the ePortfolio and in particular reflects on their prescribing using the GP prescribing proficiencies. GP trainee and their Clinical Supervisor/Trainer have a tutorial about it. Trainee creates PDP entries where appropriate.
- The trainee and GP trainer/Supervisor complete the assessment using the GP trainer/ Supervisor assessment form found in the ePortfolio
- Both the trainee and GP trainer/Supervisor complete and submit the questionnaires
- The trainee uploads the ANONYMISED spreadsheet to their learning log
For the official MRCGP prescribing tools and supporting documents to help you, see the resource items under the QUICKLINKS section at the top of the page. They are reproduced below for your convenience.
- Prescribing assessment process flow chart
- Prescribing assessment presentation
- The PRACtICe study and 100 prescription study
- Manual for GP trainee prescribing review
- GP trainee prescribing checklist /types of errors
- Examples of prescribing error and suboptimal prescribing
- Trainee self-reflection form
- GP trainer / Supervisor prescribing assessment form
- Descriptors of the assessment grades for the prescribing assessment
- Frequently asked questions
You are required to collect the data for 50 prescriptions. Many of you will be able to use the created searches below to help facilitate the gathering of the data.
- Spreadsheet for manual search (XLSX file, 39 KB)
- EMIS instructions (PDF file, 158 KB)
- EMIS video
- EMIS spreadsheet (XLSX file, 39 KB)
- EMIS search for Trainees in Scotland or where the built-in search fails (PDF file, 2.16 MB)
- File required for above search (ZIP file, 1.85 KB)
- SystmOne Instructions (PDF file, 91 KB)
- SystmOne – Further Information provided by Ardens (PDF file, 251 KB)
- SystmOne spreadsheet (XLSX file, 39 KB)
- Vision instruction (PDF file, 711 KB)
- Vision spreadsheet (XLSX file, 39 KB)
Some of you will unfortunately not be able to use this functionality, either because of the system you are using or because of how you are set up as a user on the system. If that is the case then you will need to complete this assessment by looking through all of your consultations backwards, from a particular date and identifying when you have prescribed a medication. You will then need to manually enter the information onto the spreadsheet.

Leave a Reply Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed.

