Training Diary: ST1s & ST2s in a GP Post
things to achieve before the end of your VERY FIRST 6 month GP placement (usually ST1)
- by Dr Ramesh Mehay
- Last modified: 28th October 2023
- One Comment
Quick Links
The ST1/ST2 training map (GP post)
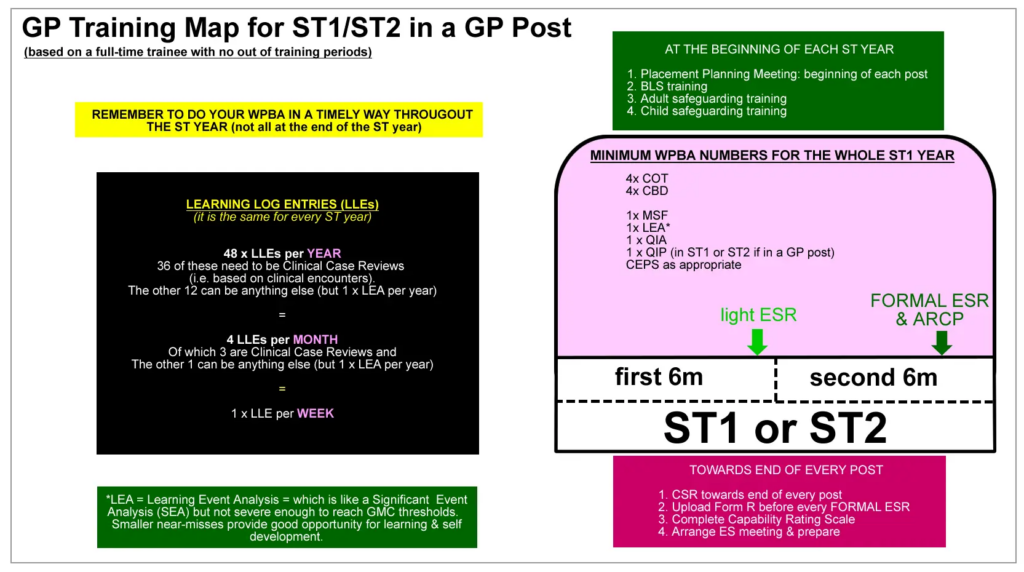
Remember, mini-CEXs are done in hospital posts only. In a GP post, do COTs instead. So, if your ST2 year is made up of 6 months of GP and 6 months of a hospital post, then by the end of that year, you will need to have done 4 x CBDs, 2 x COTs, 2 x mini-CEXs. If the whole of ST2 is hospital posts, then it is 4 x CBDs and 4 x mini-CEXs.
Broad things to achieve by end of the 1st GP post (Placement Planning meeting)
This section is good for your Placement Planning Meeting. Go through it with your GP Trainer. Everything we do as doctors and every part of our job (whether in hospital or GP) can be group into three areas which are all underpinned by PROFESSIONALISM. Those three areas are RELATIONSHIPS (which includes communication skills), DECISION-MAKING (which includes decisions on all sorts of things, including diagnosis-making) and MANAGEMENT (by management – we do not mean clinical management – we mean management in the broad sense – how we manage our work, ourselves, our sanity, our health, our personal systems, our work-personal life balance). The latter is important because happy and well-grounded doctors generally make good decisions and less mistakes. For your Placement Planning Meeting, it can be helpful to think what the trainee might want to develop in their new post in terms of these 4 areas. Click to open the items below for further clarification on each of these.
1. RELATIONSHIP SKILLS (click to open me)
What: At the end of this placement, the trainee will
- have developed good rapport with most patients. The trainee will be well on their way to developing good communication/consultation skills for face to face and telephone consultations. Not to RCA/CSA/COT standard but getting there.
- have developed and shown good working relationships with a wide variety of staff, not just the doctors.
How
- Reading a communication skills book – The Inner Consultation by Neighbour or The Naked Consultation by Liz Moulton.
- Reading a telephone consultation book.
- Through face-to-face consultations with patients.
- Practising telephone consultation skills.
- Tutorials and professional conversations with trainer and other colleagues.
- Relationship with colleagues: through day-to-day interaction with them. Showing genuine interest in other people. Demonstration in informal and formal conversations.
Output Measure:
- Face-to-Face Consultations
- Deals with the main consulting issues in face to face consultations within 15 minutes on average.
- In other words, a gradual move from 30 to 15 minute consultations.
- Adequate telephone consultations observed
- Coves the main issue and giving good advice.
- Perhaps an Audio-COT to assess more objectively (although not compulsory).
- Practice Meetings
- Contributes to practice meetings rather than just sitting back and listening.
- Demonstrates a respect for other differing opinions.
- Does not think he or she is always right.
- COTs:
- Achieving (i) Hx (ii) Ex (iii) Diagnosis (iv) Mx and (v) Patient Contribution. Always puts (vi) FU plans in place.
- Progressing in (vii) Picking Cues, (viii) Exploring ICE & (ix) PSO and (x) Explanations.
- CBDs:
- Achieving (i) Working with Colleagues and in Teams.
- Progressing in (ii) Practising Holistically and (iii) Fitness to Practise.
- MSF
- MSF comments about good relationships and working with clinical, non-clinical staff and patients.
- ePortfolio
- Log entries demonstrate thinking and reflection on specific communication micro-skills, like ICE, PSO, Signposting, Screening., Setting Agendas, Summarising, Explanations and so on.
- Log entries show good levels of reflection on feelings – of self and others.
- Log entries show an appreciation for others.
NOTE:
Achieving means trainee is achieving competence or near competence.
Progressing means although trainee might not be competent, they are progressively developing well in this area.
2. DECISION-MAKING SKILLS
What: At the end of this placement, the trainee will
- be able to deal with (i.e. make decisions on) most consultations adequately. They might still seek advice quite often, but not as much as in the beginning.
- generally make good working diagnoses, but other times will be reliant on the experienced clinical supervisor to direct them.
- be good at thinking about differential diagnoses.
- know where to look for information when they don’t know it.
- mostly develop reasonable management plans.
- know their own limits – clinically.
- know their own limits – when they are too unwell to practise safely.
How:
- Through a combination of face-to-face consultations, telephone consultations, debriefs, tutorials and professional conversations.
- Develops their own “flow diagram” of where to look for information when they don’t know it.
Output Measure:
- Debriefs
- There is gradually more and more confidence in the trainees data gathering, diagnostic, prescribing and management behaviour.
- [Note: At ST1/2 level, all patients still need to be debriefed for safety reasons – even towards the end of the placement.]
- During surgeries
- Is gradually calling less and less for help from others as their confidence grows.
- [Note – trainer/supervisor must watch out for trainees who are over-confident.]
- Other clinical practice activities
- Deals with results and letters safely.
- Can do home visits safely [all must be debriefed]
- COTs
- Achieving (i) Makes appropriate working diagnosis and (ii) Appropriate Management Plan.
- Progressing in (iii) Involving patient in decisions, (iv) Effective use of Resources.
- CBDs
- Achieving (i) Data Gathering & Interpretation, (ii) Making diagnosis & decisions, (iii) Clinical Mx.
- Progressing in (iv) An Ethical Approach and (v) Fitness to Practice.
- MSF
- Feedback from colleagues says clinical acumen is good.
- Comments about clinical management being sound.
- ePortfolio
- Log entries show good decision making skills.
- Links learning logs appropriately to Clinical Experience Groups e.g. “infants, children and young people.”
- Entries demonstrate clear evidence of learning.
NOTE:
Achieving means trainee is achieving competence or near competence.
Progressing means although trainee might not be competent, they are progressively developing well in this area.
3. MANAGEMENT SKILLS
What: At the end of this placement, the trainee will
- understand many of the different systems in General Practice.
- be able to prioritise own daily workload (both clinical and educational).
- do their admin work on time (prescriptions, referrals, letters, test results).
- be engaged in their own learning and development.
- be able to show a progression in problem-solving skills for both clinical and non-clinical problems.
- be able to recognise when they are stressed too unwell to perform.
How:
- Engages with systems like others do in the practice (clinical, non-clinical, including IT).
- Develops their own system for their daily routine work – ensuring things like test results, letters, prescriptions are done in a timely way. [Discuss with Trainer/Other GPs.]
- Dialogue with others about practice systems, safety, personal management systems and resilience. For example, in debriefs, through professional conversations and from tutorials in General Practice.
- Discussions at HDR and other workshops – on practice systems, safety, personal management systems, resilience.
- Attendance at mandatory course – BLS, ALS, Defibrillator Training, Child Safeguarding, Adult Safeguarding.
- Attendance at self-management courses.
Output Measure:
- Observed surgeries
- Uses the computer effectively in consultations.
- Uses other IT systems (e.g. ICE, pathlinks, referrals) effective in consultations.
- MSF
- No concerns over paperwork, managing tasks etc.
- Others say committed learner.
- No negative comments like shirking responsibilities.
- Educational Activities
- Prepares adequately for tutorials.
- Prepares for HDR, esp when running a session.
- Prepares for practice presentations that they may be leading on.
- Engages in Audit or other Quality Improvement project.
- CBDs
- Progressing in (i) OML, (ii) Managing Medical Complexity, (iii) Working with Colleagues (e.g. delegation, teamwork) and (iv) Fitness to Practise.
- WPBA
- Does not leave assessments until the last minute.
- ePortfolio
- Good engagement.
- Log entries entered in a timely way (not last minute).
- Log entries demonstrate evidence of learning.
- Log entries: periodically reflects on work and life to maintain a good balance.
- Most PDP items achieved.
- No concerns over sick leave taken
- Not too much and not too little.
- [Note: both too little or too much can indicate self-management problems.]
NOTE:
Achieving means trainee is achieving competence or near competence.
Progressing means although trainee might not be competent, they are progressively developing well in this area.
4. PROFESSIONALISM
What: At the end of this placement, the trainee will
- demonstrate a genuine respect for other people
- demonstrate a genuine respect for their contractual responsibilities
How
- Through everyday interactions with other people – both patients and colleagues
- Engaging with both the ePortfolio and WPBA
- Commitment to professional duties demonstrated at work.
Output Measure:
- Respect for patients
- Attends to patients in distress and discomfort.
- Nice comments from patients made to GP Trainer and others. This might be document in the MSF and CSR. Also, trainee may get thank you cards from patients for the respect and kindness they have shown.
- Shows respect for patients as individual fellow beings – in face-to-face and telephone consultations – either directly observed or recorded ones.
- Respect for work colleagues
- MSF – positive comments about the trainee’s professionalism (attitude to work, turning up on time, not shirking responsibilities, going the extra mile for patients and colleagues).
- Helps trainer/other doctors/practice during times of struggle.
- Trainee responds constructively to negative feedback from MSFs, colleagues and elsewhere.
- Shows respect for Learning Activities by planning for them.
- Prepares adequately for tutorials.
- Engages with prep for other learning activities e.g. at HDR.
- Shows respect for GP Training Requirements
- Does not belittle the ePortfolio or WPBA.
- Engages well with ePortfolio.
- Gets WPBA done and treats them with respect.
- Log entries written in a way to show evidence of learning (as opposed to non-focussed ‘waffle’ just to ‘tick a box’)
- Shows respect for the Computerised Medical Record
- by recording adequate amounts of information rather than one-liners!
- consultations added in a timely way (including home visits).
- does not falsely alter records.
- [Note to trainees: all medical systems -both hospital and GP- have an audit trail. They can tell if you have altered a medical record word by word and the exact timing! They can tell exactly what you have changed and when. So do not alter records retrospectively. Instead, add an additional note in a timely way.]
- COTs:
- Reviews own recordings and selectively tells you which consultation to look at (rather than saying “any”). This shows a respect for the assessment.
- Progressing in (i) Involving the patient, (ii) Shared decision-making and (iii) Making effective use of resources.
- CBDs
- CBD prep sheet prepared with care (as opposed to last minute quick rough-and-ready write ups). Preparation shows a respect for the assessment.
- Achieving (i) Working with Colleagues and in Teams.
- Progressing in (ii) An Ethical Approach and (iii) Fitness to Practise.
- Understands the need to ration care and protect the NHS.
- Progressively developing in this area – i.e. not over referring in a willy-nilly way, not treating every ill with a pill, and not ordering every investigation under the sun!
- Starting to consider costs and effectiveness, of tests and medication, although might not be very well polished at this stage.
Achieving means trainee is achieving competence or near competence.
Progressing means although trainee might not be competent, they are progressively developing well in this area.
The first 4 weeks
Understand the Professional Capabilities (click to open me)
The Professional Capabilities (previously called competences) are basically a set of areas YOU ARE MEASURED AGAINST. Nearly everything you do in GP Training is mapped to these 13 PCs. So, getting a real good understanding of them is crucial to you achieving them!
Understand what Log Entries are all about
One of the big things that ARCP panels and Educational Supervisors assess are your Learning Log Entries (LLEs).
You might think you know what log entries are about but trust us, it is unlikely that you truly have a grasp of what they are about or the ‘spirit’ behind them. So, rather than jumping in and writing a whole load of log entries with meaningless reams of text, slow down and try and understand the educational purpose of why we are so keen for you to do them.
These LLEs must show evidence of performance as well as learning. In other words, we want you to write log entries in a way that not only “shows us” evidence of the 13 Professional Capabilities” but also shows us that you value writing them up because of the learning revelations they reveal “for you”. Pausing for a moment, slowing down and reflecting on your clinical encounters will help you become a better doctor. The good doctor is one who continuously pauses, slows down and reflects on their behaviour and actions.
Click here to understand the basics behind Learning Log Entries
Understand the theory behind Reflection
Your log entries must show evidence of learning – in other words, that you find new revelations for yourself which then helps you to become an even better doctor.
But learning cannot happen without reflection. Therefore, understanding Reflection is a key thing to writing good learning log entries. Again, rather than jumping in to write any sort of log entry, why not learn about reflection first to help you write log entries that do “hit the mark” both educationally for you and educationally for others (like Educational Supervisors and ARCP panels).
Read Ram’s Easy Peasy Guide to Writing Learning Logs
The biggest thing that we as educators come across in GP trainees is the vast number who write up log entries so poorly. Often there is just a mere description of what happened with little analysis/intelligence behind the write up. Remember, the educators assessing your ePortfolio and log entries at ARCP time may not even know you. So you are judged according to your ePortfolio. Knowing this…
- Do you want an easy method of writing up your Learning Log Entries in a way that helps you to “showcase” yourself?
- A method that helps you provide evidence for the 13 Professional Capabilties?
- One which also helps you to reflect so that you can find and tease out those golden nuggets of key learning points that will transform the way you practice?
Then click the link below.
Don’t miss your scheme’s induction
Your induction programme run by your GP training scheme will tell you everything you need to know for your training in a nutshell. Most GP scheme induction programs run over 1-2 days . This provides a space for the TPDs to get you know you and you to know them. You will understand how GP training works in your area. It also provides a platform for to ask questions.
Please do not miss your scheme’s induction programme. It’s one of the important things for you to attend – and as early as possible. So, before your post starts, get to find out the dates (usually from your GP training scheme’s administrator). Then contact someone in your post to let them know of the dates and ask if you can book study leave for it. In a GP post, contact the Practice Manager and Trainer. In a hospital post, contact the Rota Co-ordinator and the Hospital Consultant who is your Clinical Supervisor.
The link below provides a page full of resources that many schemes will use in their Induction Programme. You may want to look at some of these just as a “heads up” sort of thing. Alternatively, you can revisit this page as a follow-up from your attendance at the local Induction Programme.
Sit in with different staff
When starting off in General Practice, it’s often mind baffling about who does what and how the whole GP structure thing work. Who can you refer to? Who are the district nurses and how do they differ from practice nurses? What can or can’t the pharmacist do? What actually happens to a prescription once it is given to a patient. What can you prescribe and what can’t you? How do the different GPs work? Do they all consult in the same way? What about the Practice Manager – what does he or she actually do? And what about the admin staff? What training do they get? What can and can’t they do? And what clinics does the surgery run? How are these organised? What on earth is QoF, CCGs, LMCs, PCNs, LES’s, DES’s, Gold standards and so on?
Well, fear not. Your induction programme should provide you an opportunity to sit in with various people and ask questions to understand “the system” better. This will include sitting in with the Doctor, Nurses, Pharmacist, Health Visitor, District Nurses, and the Midwives. You can also ask to sit on some Chronic Disease clinics held in the surgery (ask and liaise with Practice Manager). Hopefully, you will get to visit the local Pharmacist for an hour or so and see what happens to a prescription. You don’t have to sit in on the whole session – we don’t want it to become boring for you – so perhaps a 1.5 hour session will suffice.
The link below is to the GP post induction page. In the DOWNLOADS section, you will find a variety of task-sheets that you can use with different types of health professional. Use them to help you learn more about that professional rather than just sitting in, watching and getting super bored after the first hour. Instead, observe and reflect on how different health professionals consult. Ask them questions about their profession – what their qualifications are, what their training involves and what their roles are within the practice. Make notes. Discuss with your trainer.
Click here for the TASK-SHEETS for use when sitting in with different professionals
Define your daily work routine
It’s important to get a work routine going that covers all the important duties of your job as a GP. If you don’t have a routine, you’ll end up missing things and that could mean serious clinical mistakes and errors. Discuss with your GP Trainer – ask what they do to help you define yours. For example, my routine after a surgery is…
- Looking at clinical tasks
- Looking at and file clinical scanned letters
- Looking at and file blood results
- Checking physical pigeon hole
- Checking work email
And of course… Having a system of capturing and doing the tasks generated from your clinical encounters (e.g. clinical tasks)
Play with the Practice’s Medical Computer System
- Most practices use either EMIS, SystmOne or Vision. All medical systems have a “test patient” you can play with. Find out yours from your Practice Manager (PM). Ask you PM for a session with someone to help you with getting familiar with the computerised medical record.
- There are loads of YouTube tutorials – so go and find them. Watch and play around with your test patient.
- There’s also a section in the Bradford VTS Induction Handbook called “Making Friends with the Computer System”. The last two pages of the handbook.
- Practices may often have add on computer systems like ARDENS and ASSIST – ask if your practice has any of these. Again, get one of the doctors to show you how to use these. Or look up tutorials on YouTube first.
If you’re not good with typing – NOW is the time to learn. You will not survive General Practice if you can’t type very well. Everything is done electronically these days.
- Learn how to type with TypingClub.com
- I also like “Mavis Beacon Teaches Typing” software, available from Amazon.
Play with your ePortfolio
Log into FourteenFish and start getting familiar with the layout. Simply log in 3-4 times a week for the first 2 weeks just to get a feel for it. It takes a while to get used to it. Then, when the time is right for you to start adding stuff, it won’t be such a headache and you’ll find it nice and easy. It’s horrible writing up things like Learning Log Entries if there is the added problem of not knowing where to click or which buttons to press. So, get rid of that unnecessary burden by simply getting used to the system in the first couple of weeks of your post without the pressure of having something to add.
Does your English need improving?
This mainly applies to those of you who qualified in medicine from a country outside of the UK. You decided for yourself by asking yourself – “Do I need to improve your spoken English?”. If yes, then how will you do it? Make a plan to start doing it in ST1, so that by the time it comes to the start of ST3 (i.e. 2 years later), you will have improved significantly for you to pass the exams like SCA where your level of English fluency is so critically important. And seeing patients and dealing with them is so much easier when you easily understand what they say, you easily express yourself, and you easily make a plan together. You need to “live, eat and breathe” English – which means if you speak English when at work but the rest of your life is in your native home language (i.e. 60% or so), then you are are not going to improve your English rapidly. Find opportunities to converse in English OUTSIDE of the workplace too.
So, consider a combination of….
- Watching a TV series in English
- Listening to audiobooks – some examples below
- Watching your favourite movies again but this time in English
- Speaking to your children at home in English,
- Attending a Language School/Class (search on MeetUp App or search online for something local)
- Finding a language teacher or native friend to help you on a 1-1 basis.
- If your part of a group like “The Sudanese SCA group”, then consider asking people to speak in English rather than Sudanese or Sudanese Arabic.
One good method, in terms of conversation, is to try and speak opportunistically to as many people in English as you can every day. Make notes on your areas of difficulty and discuss with either your English language teacher, GP trainer, a English friend or relative. Another good way is for your friend or teacher to listen to you while you read them a story book – and they correct you as appropriate. Pick one of the following books and see how you get on. These are all great “story style” books written by authors who are medical doctors. You will also hopefully learn some of the wisdom from the experiences of these doctors.
- This is Going to Hurt: Secret Diaries of a Junior Doctor – by Adam Kay.
- The Doctor Will See You Now by Amir Khan
- Complications OR Better by Atul Gawande
- SeaSickness by Peter Tate
- The Inner Consultation by Roger Neighbour (you learn two things – medical communication skills and language skills)
Once you have developed a plan – make sure to do it regular – e.g. every Tues 6-8pm.
Join Bradford VTS Learning Circle - it's FREE
The first 3 months
Plan your courses in advance
Do remember that although you’re a GP trainee, you are also an employee who is paid to do a job. Although you will be entitled to study leave, that doesn’t mean you can just take it when you like. It has to be co-ordinated. Hospital departments and GP practices have a service to deliver to patients. Therefore, they can’t just release you at the drop of a hat for you to attend a course that you have booked at the last minute. So, book your training courses with plenty of advance notice (at least 6 weeks), including the induction course run by your GP training scheme. Courses to consider at this stage are:
- BLS course
- Adult & Child safeguarding courses
- GP knowledge update course as run by NB Medical or Red Whale
- Specific knowledge based course – e.g. family planning/contraception, child health, reading ECGs, spirometry, COPD, diabetes
- Urgent & Unscheduled Care course (to help prepare for Out of Hours work)
- Consultation Skills training course
- Courses targeting IMGs (if you’re an IMG)
Start reading a consultation book
Reading a book on Communication and Consultation Skills will really help you harness the power of effective communication in gathering clinical information quickly. This will then help you with making good decisions, and explaining things to patients in a way that is acceptable to them. Communication skills also help enormously when things go wrong. And of course, they are crucial for the COT assessments and CSA exam.
If you like reading novels, we suggest
- The Inner Consultation by Roger Neighbour. An old classic, but still relevant today with a great story-telling narrative. [Paperback] [Kindle]
- Bedside Matters by Peter Tate and Francesca Frame. Conversational in style and has great reviews and written in 2020. [Paperback] [Kindle]
If you prefer straight to the point books, we suggest
- “The Naked Consultation” by Liz Moulton. A great all-rounder. Covers difficult situations. [Paperback] [Kindle]
- “The Modern Guide to GP Consulting” by Alex Watson. Six S for Success. Straight to the point and easy to read short book. [Paperback] [Kindle]
- “Consulting in a Nutshell” by Roger Neighbour. Neighbour’s latest book written in 2020, gives a 3 step approach to the consultation. Also sections on how to handle difficult situations. [Paperback] [Kindle]
- The GP Consultation Reimagined – a tale of two houses by Martin Brunet – a creative way of thinking about the consultation. [Paperback] [Kindle]
If you don’t know which of the above books to go for… head over to Amazon – and read the synopsis of each book and the accompanying reviews. Then simply pick one that grabs your fancy. To be honest, they are all pretty good. You may have heard about the book “Skills for Communicating with Patients” by Silverman et al – It is a great book and one of our favourites – because it’s the only evidence-based communication skills book out there and is VERY practical. But is heavy going for ST1s or ST2s, so, best reserved for ST3s. Please buy through our Amazon Affiliate links above. We only get 4% but every little bit helps to keep this site free.
Remember your ePortfolio
By now, you should be doing around 1 log entry per week. Please get your GP trainer to look at these and see how they fair in terms of reflection, learning and evidence for the capabilities. Get your GP Trainer to show you how you can write them in a more reflective and educational way. For example, by using the ISCE criteria to write your log entries, you can end up creating more powerful learning moments for you.
- I for enough Information about the situation,
- S for Self-awareness and describing how the situation made you feel and any accompanying thoughts,
- C for doing some Critical analysis to make sense of the situation
- E for Evidence of learning – i.e. showing exactly what needs to be done/change in behaviour to make you or the system you operate in better.
In terms of numbers…
- 1 log entry per week.
- In other words, 4 log entries per month.
- 3 of these need to be on a clinical encounter with a patient (and recorded under Clinical Case Reviews).
- The other one can be on anything you like – for instance, writing up a HDR session and reflecting.
- You could make it easy for yourself and decide the last week of every month will be a log entry on “something else like HDR”. All others will be Clinical Case Reviews
Understand WPBA + do a COT & a CBD
Start to read and get familiar with all the different types WPBA. Almost everything you would want to know (plus hints and tips not available anywhere else) can be found on this Bradford VTS website – under main menu of our website.
Bradford VTS HOMEPAGE > Main Menu > GP TRAINING & MRCGP > WPBA
Click here for an intro to WPBA
How to Study
Isn’t it interesting that most of us are never taught “how to study”. Yet the research says there are numerous methods – some more highly effective than others. In fact, some of the methods we think are good are in fact wasteful ineffective methods that consume a lot of time and energy for little effort.
Over the next 2-3 years, you will be learning a lot of new things. Not only that, but you will do some exams to demonstrate your knowledge and skills. Therefore, it is probably a good time to start reading up about some of the research around “how to study effectively” so that you can change any bad habits and adopt some new ones. Doing this in ST1 – which is probably the easiest of all the three years – is therefore the ideal place to do this.
Read the research on Bradford VTS on what makes effective Studying. Discuss it with your trainer and/or Educational Supervisor or TPD. Summarise the key learning points that you will implement (and even record it as an ePortfolio learning log to demonstrate evidence for the capability Performance, Learning & Teaching).
Think about doing a teaching session for HDR for your colleagues
Some trainees think that teaching is easy – you just get up and do it. But effective teaching requires a lot of effort and skill on the part of the teacher. Take your GP Trainer – did you know that he or she has been on numerous courses to learn not only some theories around what makes effective teaching and learning but also demonstrate they have the practical skills to do it? Not only that, but they have to keep showing that they are maintaining their educational skills by being revalidated every few years. So, your GP trainer is a highly skilled educator.
So, if you plan to do or have been asked to do a teaching session – perhaps at HDR, at a GP or hospital team meeting, why not take the opportunity and learn some basic teaching skills. This is a lot better than just trying to copy what “you think” is good from what you have observed in other teachers around you. If you learn some of the theory NOW, you will understand what exactly you are doing on an educational level. It will also help you understand why some teachers are more effective than others. Have a look at these…
The good (effective) teacher or teaching. What does the evidence say?
Don’t forget to visit Bradford VTS often
And finally, there are tonnes of other things on this website. We have over 2000 resources. But please don’t feel overwhelmed. You have 3 years to dip in and out of this website and learn things gradually and in a relaxed way. The purpose of this site is to demystify GP training and use easier language than the RCGP website to help explain things in a more meaningful and practical way.
And of course, there are tonnes of things like help sheets and training material that you simply cannot find elsewhere. It’s mostly free too! There may be a small charge for the odd thing here and there, primarily to help raise funds to keep this site alive. Please support us through a voluntary contribution, buying from our book store etc. We also have a lot of online resources which are accessible through the main header of this site. Please get in touch if you would like to help update these and get your name published on Bradford VTS (good for your CV) – rameshmehay@googlemail.com
Click here to see our ONLINE VIDEO LIBRARY – please get in touch if you would like to do some videos yourself (I will guide you) and get your name published on Bradford VTS (good for your CV) – rameshmehay@googlemail.com. Also, don’t forget to subscribe to our YouTube channel.
ONE FINAL THING… We love providing information on this website for free. We put a lot of work in. To help keep it free, please give us a little donation to keep it going. If you love it, please give something back. We are not out to make a big profit, but just cover our costs and play with new technology (which costs money – so please give us some!). Even something as small as £30. Please pledge a small something. We do all of this in our spare time.
Click image for physical version & text for Kindle. Please 🙏🏽buy through our Amazon Affiliate link. We only get 4%, but every bit helps to keep this site free for you. 🥰🧡😍
The last 3 months
How is your ePortfolio going?
If it is going badly, try and work out why and discuss it with your trainer. Perhaps you need more training with your trainer on how to write a good learning log entry. Learning log entries should not only provide evidence for the capabilities, but they should also be an rewarding educational experience for you. If this isn’t the case, discuss with your GP Trainer.
Your ePortfolio is one of the main things that is used in all your assessments like ES and CS meetings, and ARCP panels. So it is right that you should pay a lot of attention and respect to it. Write things carefully – concisely – to demonstrate evidence – to show learning – rather than lengthy write ups of mindless waffle. Remember, there should be 4 log entries per month. 3 of these need to be on a clinical encounter with a patient (and recorded under Clinical Case Reviews). The other one can be on anything you like – for instance, writing up a HDR session and reflecting.
In terms of WPBA – get at least the minimum number of things like CBDs, COTs and CEXs – in fact you should aim to get a lot more! And make sure you do them in a timely way – throughout the post, not all done at the end as a desperate last measure. Remember, your GP Trainer will NOT remind you when these are to be done. The responsibility is yours to ask your trainer to do them – because we are trying to get you to become an autonomous learner, where you don’t need your hand holding!
Do another COT & CBD
- Time to do another COT and a CBD. By the END of ST1 you need to have done a minimum of 4 x CBDs and 4 x COTs. That means x2 of each in the first post and x2 in the second.
- Remember, COTs are done in GP posts only. In a hospital post, do mini-CEXs instead. So, if your ST1 or ST2 year is made up of 6 months of GP and 6 months of a hospital post, then by the end of that year, you will need to have done 4 x CBDs, 2 x COTs, 2 x mini-CEXs.
- However, demonstrate that your more than just an “average” GP trainee – try and get more than this MINIMUM number.
Click here to revisit the intro to WPBA page
Time to do a QI Project
Yes, you need to do a Quality Improvement (QI) project before you finish ST1. It is a mandatory requirement. Non-negotiable! This is because GPs are the main driving force behind changes and improvements in health care systems. And we cannot just sit on our seats and carry on doing what we have always done. Clinical knowledge and discoveries are happening at a phenomenal rate and we must keep up in order to serve our patients with good quality health care delivery in keeping with the latest evidence and research. Wouldn’t you agree?
So, now is the time to think of some ideas. Discuss with your Trainer. Don’t pick anything too complicated. Keep things simple. And of course, you will enjoy it more if you pick an area you find most interesting.
- Click here to go out our page on the Theory behind Quality Improvement
- For the different types of QI projects you can do – we have examples and advice of them all – under our home page simply click “QI, PROJECTS, EBM & STATS”
Are you working on your PDPs?
Every GP Trainee needs to write some PDPs for every post they start. Why? Because when you qualify as a GP, you will do the same every year! A PDP is a Personal Development Plan – usually consisting of 3-5 things that you want to achieve to help you be even better than you currently are. In this way, every GP becomes incrementally better year-on-year. The needn’t be big things, but they should make a difference to your working life. So, for instance, if you feel your general clinical knowledge is good except for in contraception and family planning, then you may want to book onto a workshop or course on that. Sometimes a PDP might be achieving a better work-home life balance. Achieving a better balance makes us happier and happier doctors always perform better than sad grumpy ones!
The basic rule for defining a PDP is that they should be “SMART”. If they are “SMART”, they are more likely to be achievable. SMART means..
- S for being Specific which what you are trying to achieve (e.g. ‘improve my knowledge of contraception’ rather than ‘improve my clinical knowledge’)
- M is for the thing you want to achieve being Measurable (e.g. attendance a course).
- A is for Attainable – in other words, what you plan to do is do-able and not something almost impossible. “attend a course on consulting skills” is do-able. “read 10 different books on consulting skills” is incredibly difficult.
- R is for Realistic. For example, “read a consultation book before the end of next week” is difficult. “Read a consultation book over the next 3 months” is realistic.
- T is for Time–bound. In other words, you define the time period over which you will achieve what you set out to do.
Are you engaging with UUC
UUC stands for Urgent Unscheduled Care and experience for this is mostly gained through being the on-call duty doctor for your surgery during normal working hours AND/OR as the emergency doctor for the local Out-Of-Hours (OOH) centre.
During ST1 you should be mostly observing other qualified GPs doing it and perhaps seeing a few patients – but directly supervised.
Check with your Training Programme Administrator if you need to do OOH and if so, how many sessions and how to book on. There will be a local system in place. If you have a contractual duty to do a certain number, then that contractual duty is mandatory. Don’t forget to write up about your experience in UUC (to provide evidence for it).
Good Practice Guidance for doing UUC
- Do no do all your OOH/UUC in the last GP post – not only is this unacceptable (and shows poor time management and organisation skills) but also will prove to be VERY stressful for you. You will have a big list of things to do when in ST3 (on top of the GP exams!).
- If you do an OOH session, you need to tell the practice because you need time off to ensure you do not break the 40h per week working time limit.
- When writing them up in your ePortfolio – try and a brief list of patients seen and reflect on the OOH session in terms of ONE OR MORE of the UUC Capabilities.
Get ESR & CSR done
Please take your Educational Supervision (ES) sessions seriously. The assessment and outcome of these ES meetings feed into the ARCP panels which determine whether you have made good progress to enable you to proceed onto the next ST year.
There have been many instances where trainees have not been allowed to progress and instead repeat part of their ST year because of poor educational or clinical performance. Remember, the only judgement the ARCP panels make of you is based on your ePortfolio. And many of the people on those panels will NOT know you as a person. They have only your ePortfolio to judge you. And the Educational Supervisor will make and assessment of your ePortfolio also and the panel will look at the ES report.
So, make your ePortfolio look good, and prepare well for your ES meeting. Expect your ES meeting to last 2-3 hours. There are 3 sections of your ES prep form to pay a good detailed amount of time
- “FINDING THE EVIDENCE FOR THE CAPABILITY SELF-RATING SCALES”.
- “FORMULATING ACTION POINTS FOR THE CAPABILITIES”
- “PDPs”
We have advice for both of these in the links below.
Also ask your GP trainer to fill out a CSR – Clinical Supervisor’s Review.
- Click here to access our Educational Supervision pages which tell you how to prepare.
- This page tells you how to write up “The Evidence for the Capability Self-Rating Scales”
- This page tells you how to “FORMULATE ACTION POINTS FOR THE CAPABILITY AREAS”
- This page tells you everything you want to know about PDPs
- Want to learn more about ARCP panels? Click here.
How to Study
Isn’t it interesting that most of us are never taught “how to study”. Yet the research says there are numerous methods – some more highly effective than others. In fact, some of the methods we think are good are in fact wasteful ineffective methods that consume a lot of time and energy for little effort.
Over the next 2-3 years, you will be learning a lot of new things. Not only that, but you will do some exams to demonstrate your knowledge and skills. Therefore, it is probably a good time to start reading up about some of the research around “how to study effectively” so that you can change any bad habits and adopt some new ones. Doing this in ST1 – which is probably the easiest of all the three years – is therefore the ideal place to do this.
Read the research on Bradford VTS on what makes effective Studying. Discuss it with your trainer and/or Educational Supervisor or TPD. Summarise the key learning points that you will implement (and even record it as an ePortfolio learning log to demonstrate evidence for the capability Performance, Learning & Teaching).
If you plan to do a teaching session…
Some trainees think that teaching is easy – you just get up and do it. But effective teaching requires a lot of effort and skill on the part of the teacher. Take your GP Trainer – did you know that he or she has been on numerous courses to learn not only some theories around what makes effective teaching and learning but also demonstrate they have the practical skills to do it? Not only that, but they have to keep showing that they are maintaining their educational skills by being revalidated every few years. So, your GP trainer is a highly skilled educator.
So, if you plan to do or have been asked to do a teaching session – perhaps at HDR, at a GP or hospital team meeting, why not take the opportunity and learn some basic teaching skills. This is a lot better than just trying to copy what “you think” is good from what you have observed in other teachers around you. If you learn some of the theory NOW, you will understand what exactly you are doing on an educational level. It will also help you understand why some teachers are more effective than others. Have a look at these…
The good (effective) teacher or teaching. What does the evidence say?
Don’t forget to visit Bradford VTS often
And finally, there are tonnes of other things on this website. We have over 2000 resources. But please don’t feel overwhelmed. You have 3 years to dip in and out of this website and learn things gradually and in a relaxed way. The purpose of this site is to demystify GP training and use easier language than the RCGP website to help explain things in a more meaningful and practical way.
And of course, there are tonnes of things like help sheets and training material that you simply cannot find elsewhere. It’s mostly free too! There may be a small charge for the odd thing here and there, primarily to help raise funds to keep this site alive. Please support us through a voluntary contribution, buying from our book store etc. We also have a lot of online resources which are accessible through the main header of this site. Please get in touch if you would like to help update these and get your name published on Bradford VTS (good for your CV) – rameshmehay@googlemail.com
Click here to see our ONLINE VIDEO LIBRARY – please get in touch if you would like to do some videos yourself (I will guide you) and get your name published on Bradford VTS (good for your CV) – rameshmehay@googlemail.com. Also, don’t forget to subscribe to our YouTube channel.
ONE FINAL THING… We love providing information on this website for free. We put a lot of work in. To help keep it free, please give us a little donation to keep it going. If you love it, please give something back. We are not out to make a big profit, but just cover our costs and play with new technology (which costs money – so please give us some!). Even something as small as £30. Please pledge a small something. We do all of this in our spare time.
And have you joined Bradford VTS Learning Circle? If not, why not? You’re missing out!

It’s all now fixed