Diabetes
Bradford VTS Clinical Resources
- by Dr Sabah Malik
- Last modified: 26th January 2024
- No Comments
DOWNLOADS
path: DIABETES
WEBLINKS
PATIENT LINKS
……………………………………..
Information provided on this medical website is intended for educational purposes only and may contain errors or inaccuracies. We do not assume responsibility for any actions taken based on the information presented here. Users are strongly advised to consult reliable medical sources and healthcare professionals for accurate and personalised guidance – especially with protocols, guidelines and doses.
COME AND WORK WITH ME… If you’d like to contribute or enhance this resource, simply send an email to rameshmehay@googlemail.co.uk. We welcome collaboration to improve GP training on the UK’s leading website, Bradford VTS. If you’re interested in a more active role with bradfordvts.co.uk (and get your name published), please feel free to reach out. We love hearing from people who want to give.
……………………………………..
Diabetes at a Glance
SYMPTOMATIC
Symptoms of hyperglycaemia (polyuria /polydipsia, unexplained weight loss. visual blurring, genital thrush, lethargy) plus either:
HbA1c: 48mmol/mol or higher (LAB TESTING) (Type 2 diabetes is diagnosed in adults who are not pregnant and do not have haemoglobinopathy or haemolytic anaemia by a glycated haemoglobin (HbA1c) level of 48 mmol/mol or above.
The WHO state that diagnosis should be confirmed with a repeat HbA1c test, unless clinical symptoms and plasma glucose levels >11.1mmol/l are present in which case further testing is not required.)
FBG: >7.0mmol/L or higher x2
Dip urine to check for ketones
ASYMPTOMATIC
In the absence of symptoms – 2 abnormal results on separate days are required for the diagnosis.
Results:
- HbA1c > 48 mmol/l → repeat HbA1c test after 2 weeks → if HbA1c >48 mmol/l then code Diabetes and set recall
- HbA1c 42-47 mmol/l → code and set “at risk of diabetes” recall
May not be accurate in the following cases:
- ALL symptomatic children and young people
- Symptoms suggesting Type 1 diabetes/pancreatic insufficiency (any age)
- Short duration diabetes symptoms
- Patient at high risk of diabetes who are acutely ill
- Taking medication that may cause a rapid glucose rise e.g steroids, antipsychotics
- Acute pancreatic damage/pancreatic surgery
Patients with haemoglobinopathy – the labs test for this and will detect abnormalities.
A diagnosis of diabetes has important legal and medical implications for the patient and it is therefore essential to be secure in the diagnosis.
A diagnosis should never be made on the basis of glycosuria.
A stick reading of finger prick should be confirmed by a venous sample, as per NICE guidelines.
- > 40 years of age with two or more of the following;
- family history in a first degree relative,
- BMI >25
- South Asian ethnicity
- screen at least every 5 years with a fasting blood sugar.
- Women with a history of gestational diabetes (annual screening)
- Hypertensives (annual screening)
- Patients with ischaemic heart disease, peripheral vascular disease or stroke (annual screening)
- Symptoms
- Polydipsia, polyuria/nocturia, weight loss & fatigue (typical diabetes symptoms)
- recurrent UTIs
- recurrent skin infections
- recurrent thrush
- neuropathic symptoms
- changes in visual acuity
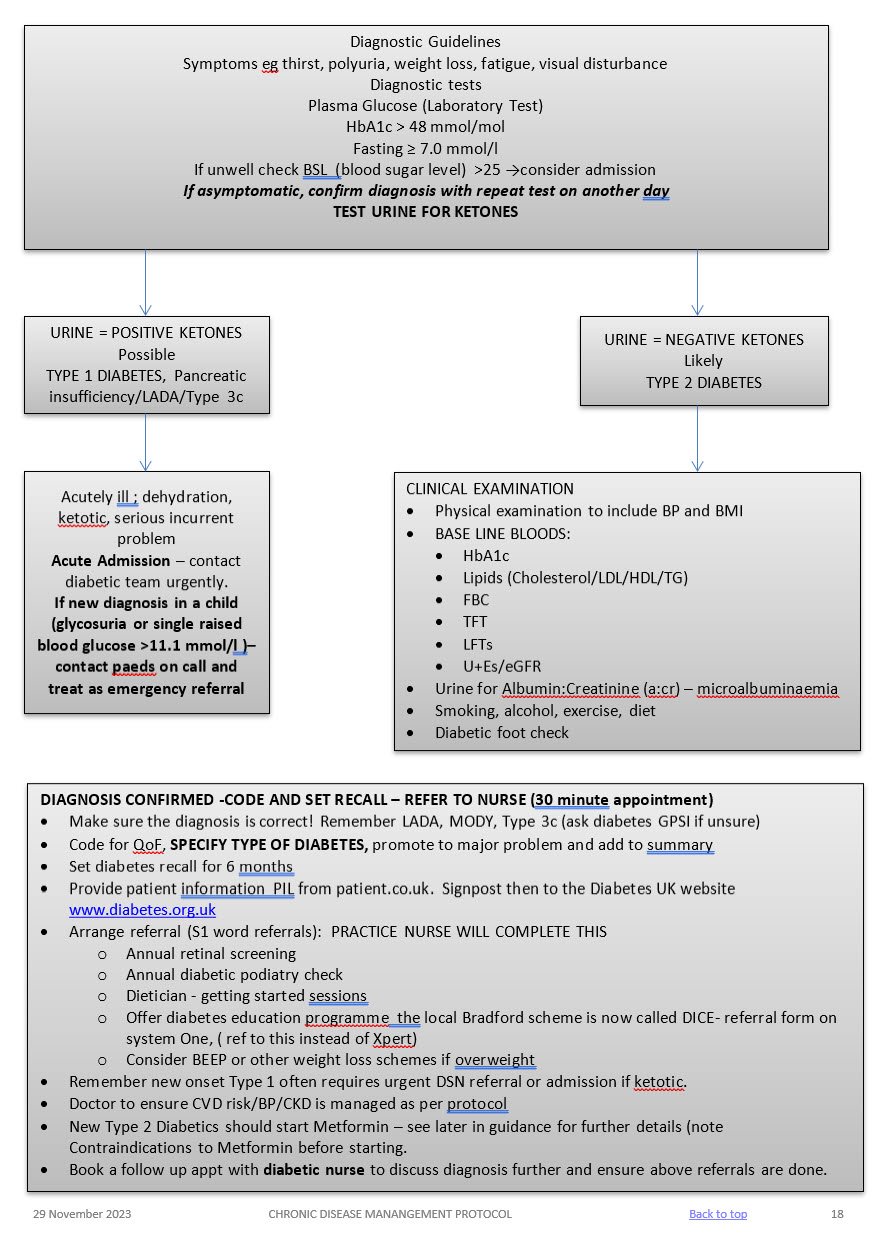
Admission
Admit to hospital if the person is at risk of a hyperglycaemic emergency (vomiting, abdominal pain reduced conscious level, heavy ketonuria, dehydration requiring IV fluids, hypotension, and serious intercurrent problem).
Same day referral
Refer to be seen on the same day if the patient is acutely ill, consider Type 1 Diabetes/pancreatic insufficiency if ketonuria present, the patient is slim and has a short history of marked symptoms (weight loss, thirst, and polyuria).
Early Referral
Diabetes and pregnancy requires referral to the hospital diabetes team
LIFESTYLE
BMI
Aim for healthy BMI <25 – consider dietition, Orlistat, other dietary measures & EXERCISE
ALCOHOL
Not to exceed recommended limits. (14 units men and women)
SMOKING
Stop!
BLOOD PRESSURE
Active management is essential!
Over half of all diabetics are hypertensive. Trials have shown that excellent BP control reduces retinopathy, nephropathy, strokes, heart failure and MI. BP control is as important as glycaemic control! TARGET < 130/80
Treatment
- 1st line – ACEi, ARB if they cannot tolerate it.
Ramipril starting regime derived from the HOPE study regime and BNF guidelines
If U&Es pre treatment reveal a creatinine < 150 micromol/l and a sodium >130 mmol/l then 2.5 mg Ramipril daily (1.25mg if on lower dose concomitant diuretics) for one week with check U&Es and an increase to 5.0 mg Ramipril for a further two weeks. Re-check U&Es and if indicated increase to 10mg Ramipril and repeat U&Es at least on an annual basis. If eGFR falls > 25% or creatinine rises by > 30% stop or back titrate treatment – see NICE guidelines. Don’t forget BNF cautions and contraindications. - 2nd line – CCB or, thiazide like diuretic or, Beta blocker (especially if there is a history of ischaemic heart disease),. Follow hypertension protocol
LIPIDS AND CVD RISK (see lipid modification protocol)
Offer generic Atorvastatin 40mg (Bradford Healthy Hearts) if their Q risk >10% (aged between 18-84 yrs), have been diabetic for > 10 years or, over 40 years old. Target chol <4mmol/l
For diabetics with established CVD offer secondary prevention or Chol > 4mmol/l – Atorvastatin 80mg
Triglycerides:
If TG level remains high (above 4.5mmol/l) please ref to CKS guidance on lipid modification or in-house lipid modification protocol.
Do not routinely offer Nicotinic acid or Omega fish oils.
MICROALBUMINURIA AND CKD
- All diabetics need testing annually for microalbuminuria and eGFR – microalbuminuria is the first sign of diabetic kidney disease and occurs before eGFR falls.
- SEE CKD PROTOCOL
ANTIPLATELETS
- Do not offer anti-platelets unless there is evidence of CVD
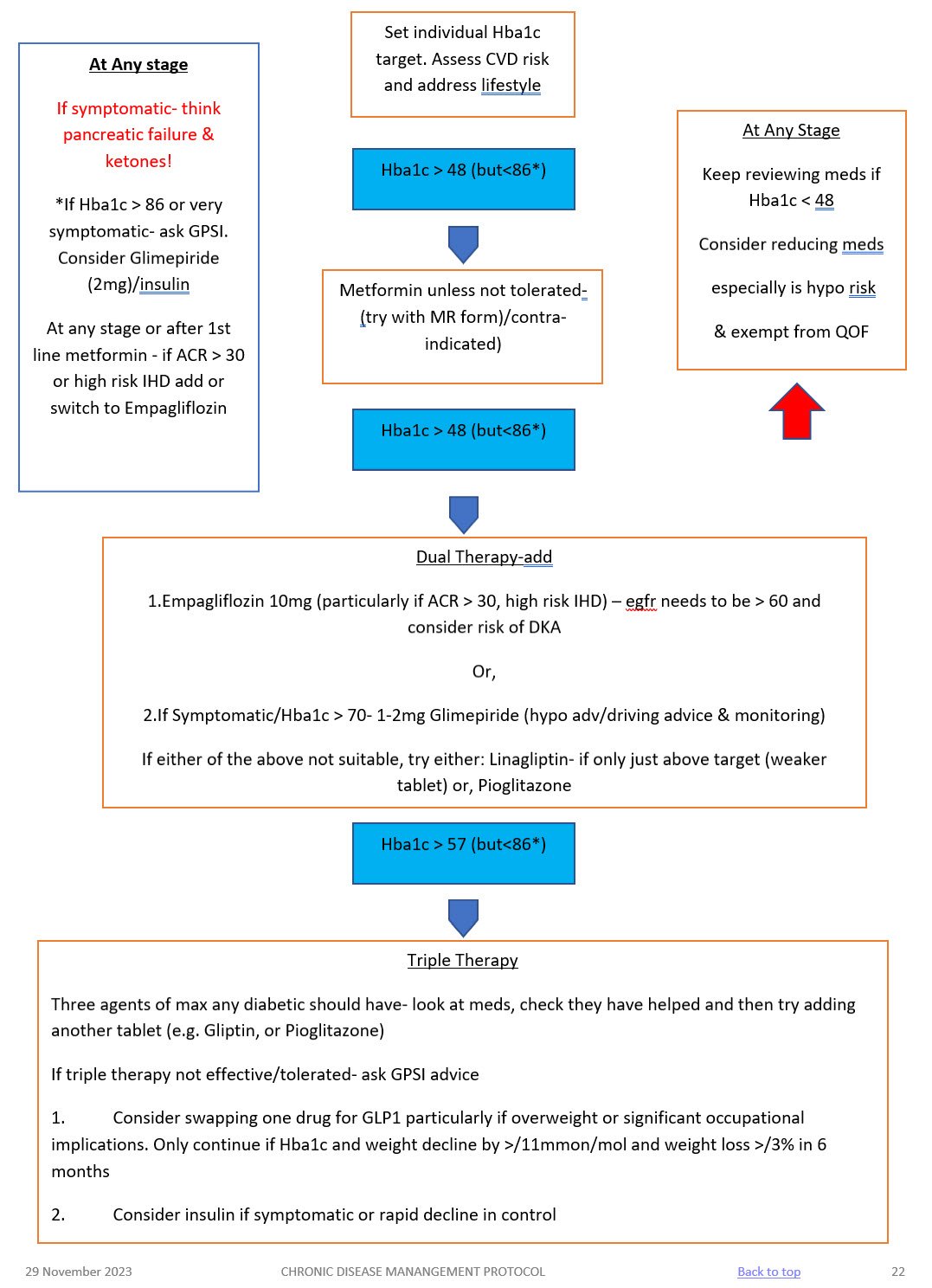
NICE recommended Hba1c targets are:
- 48mmol/mol – people who are managed by lifestyle and diet
- 48mmol/mol – people who are managed by lifestyle and diet combined with a single drug not associated with hypoglycaemia (such as metformin)
- 53mmol/mol – people who are taking a drug associated with hypoglycaemia (such as sulphonylurea), combination treatment
See table below for suggested targets for frail/elderly patients. Please exempt from QoF if you follow these targets putting an explanation in the notes.
Hba1c Target: aim for 48mmol/mol (if on diet or single drug not affected by hypoglycaemia ) or <53mmol/mol (if on SU, or more than one medication). Caution: elderly
- Start Oral treatment usually Metformin at diagnosis. Metformin 500mg ideally with evening meal, increasing to 1 gram a week later if they have no side effects.
- Please remember Metformin is very effective, reduces cardiovascular risk, retards weight gain and is not usually associated with hypos – but is contra-indicated if Creatinine > 150 (or eGFR < 40) in CCF or significant hepatic dysfunction.
- Metformin has to be stopped if eGFR fall below 30!
- Metformin MR can be used if they run into problems with GI side effects.
- Don’t forget that on starting hypoglycaemics to complete the prescription exemption form for those patients under 60 years of age.
- If you are starting a sulphonylurea (ideally Glimepiride) – ensure they are counselled and documented about:
- symptoms of hypos
- hypo management
- hypos and driving and remind them about informing their car and travel insurer AND document this in their records. If they hold HGV or PSV license then check with the 6 monthly updated DVLA guidance with respect to them having to inform the DVLA.
- Ensure they have been given a glucometer and a sharps bin, test strips and lancets are added to their repeat prescription
- DISCUSS AKI SICK DAY RULES ADVICE – see hypertension protocol for full advice.
FUNCTIONALLY DEPENDENT
- Due to loss of function, having impairments of ADLs
- Increased likelihood of requiring addition medical &/or social care
- HBA1c target: 53 – 64mmol/mol
FRAIL
– Combination of significant fatigue, recent weight loss, severe restriction in mobility & strength, increased propensity for falls & increased risk of institutionalisation
– A recognised condition & accounts for 25% of older people with diabetes
– Clinical Frailty scale or CHSA 9-point scale (assessment tool)
– HBA1c target: 60-70mmol/mol
DEMENTIA
– Degree of cognitive impairment leading to sig. Memory problems, a degree of disorientation, or a change in personality & unable to self care
– MiniCog tool (easy to use assessment tool)
– HbA1c target: 60-70mmol/mol
END OF LIFE CARE
- Significant illness or malignancy & have life expectancy reduced to <1 year
- Glycaemic aim – hypo and symptomatic hyperglycaemia avoidance
Medication | Mode of action | Side effects | Cautions (check BNF for more detail) | Dose |
METFORMIN 1st line treatment, unless BMI <25 (23 in South Asian population) Low Hypo risk Reduces CVD risk, weight neutral | Helps to stop the liver producing new glucose. It helps to overcome insulin resistance by making insulin carry glucose into muscle cells more effectively.
| Main side effect if GI affects, generally dose dependent-can be reduced with gradual increase in dose over several weeks or trying modified release Metformin Also: metallic taste, reduced absorption of vitamin B12, build up of lactic acid in the blood, allergic reaction and liver problems. | STOP/DO NOT USE IF eGFR <30 ml/min *Lactic acidosis- care if eGFR < 45ml/min. Document that advice has been given to stop these tablets if they become dehydrated (restart when eating normally again) *GI side effects. Titrate dose slowly to reduce side effects NOTE IF ALT> 3 TIMES NORMAL | Start at 500mg ideally with evening meal, increasing to 1g with evening meal after a week if they have no side effects. Max dose 2 gram over 4 weeks. Consider slow release for to reduce tablet load or if they are struggling with GI side effects.
|
SGLT-inhibitor Empagliflozin Low hypo risk Can help with weight loss | Sodium-glucose co-transporter 2 (SGLT2) inhibitor that prevents glucose reuptake in the kidney, leading to the excretion of excess glucose in the urine. | Polyuria, polydipsia, thrush. UTI, fluid depletion Increased risk of amputation- avoid if h/o leg ulcers | Only start if Cr Clearance > 60. Care if > 75 years. Risk of postural hypotension. Care needed if they have skin ulcers – risk of amputation. Document advice about normoglycaemic ketoacidosis and give ketostix. | Empagliflozin 10mg. Can be increased to 25mg. Expensive so only continue if there is a clear response after 6 months |
SULPHONYLUREA (SU) Glimepiride Risk of hypos Good if rapid response is needed. | They work by stimulating cells in the pancreas to make more insulin. They also help insulin to work more effectively in the body.
| Weight gain. Hypoglycaemia, gastrointestinal side effects, low sodium, facial flushing and intolerance of alcohol, allergies etc.
| Can cause hypoglycaemia, particularly if there is renal impairment or they are elderly. Consider occupation – hypos if not eating regularly, fasting. Make sure you give and document advice about hypos. Make sure they are able to test their blood glucose – issue glucometer, test strips, lancets and sharps bin. (SGBM) Document advice about driving/insurance. | Start at 1mg and titrate up to 4mg depending on glucose level. Should have an effect on Hba1c over a 2 month period. |
GLIPTIN Do not cause weight gain and encourages patient satiety. Although they probably reduce Hba1c levels less than other drug treatments. Low hypo risk | They work by blocking the action of the enzyme, DPP-4, which destroys the hormone Incretin.
| Gastro-intestinal effects, oedema, headache, Avoid if h/o Pancreatitis or heart failure or liver problems. | *Expensive- only continue if they meet NICE guidance. *Not v powerful max likely reduction ~ 11 mmol/mol *Do not use if a h/o pancreatitis *Monitor egfr at reviews *Don’t use if heart failure risk | Linagliptin 5mg if eGFR < 50 |
GLITAZONE Pioglitazone Low hypo risk Consider in people with very significant features of metabolic syndrome. South Asian | Reducing insulin resistance. Improving insulin sensitivity.
| Oedema esp if heart failure or at risk. Rare reports of liver dysfunction. Weight gain, gastro-intestinal side effects, headache, dizziness.
| Discuss with member of Level 2 team before starting. Avoid if they have heart failure or risk of fluid overload Avoid if h/o bladder cancer, undiagnosed haematuria Avoid if fracture risk Monitor LFTs at each diabetic review. Annual urine dip looking for haematuria | Pioglitazone:15mg-30mg. A six month period may be needed to really see an effect from these tablets. NICE recommends that they are only continued if at least a 11 mmol/l reduction in Hba1c is seen within 6 months of starting the treatment.
|
GLP-1 mimetic/insulin | Discuss with Level 2 doctor |
|
Metformin & eGFR
- If eGFR>45 – can use metformin up to max dose 1g bd
- If eGFR lower than this, risk of lactic acidosis
- If eGFR<45 – reduce metformin to 500mg bd
- If eGFR<30 – stop metformin.
- At first warning of episode of hypoglycaemia:
- Immediately treat with a 15-20g of a short-acting carbohydrate such as:
- 200 mls of Lucozade (please note Lucozade formula has changed so lower in sugar- need 200ml)
- 200mls of non-diet drink
- 4-5 glucose tablets
- 3-4 jelly babies
- 200mls of fruit juice
- Immediately treat with a 15-20g of a short-acting carbohydrate such as:
- If the hypo is more severe, and the patient cannot treat themselves:
- applying Glucagel (or treacle, jam or honey) on the inside of cheeks and gently massaging the outside of cheeks.
- if unconscious, Glucagon can be injected if the person treating has been trained to use it.
- Otherwise call an ambulance immediately
- Important:
- If unable to swallow or unconscious, do not give anything by mouth (including Glucagel, treacle, jam or honey). Make sure family and friends are aware of this. If unconscious, place patient in the recovery position (on side with head tilted back) so that tongue does not block throat.
- Follow-on treatment:
- To prevent blood glucose levels dropping again, follow sugary foods with 10-20g of a longer-acting carbohydrate such as:
- half a sandwich
- fruit
- a small bowl of cereal
- biscuits and milk
- the next meal if due
- Patients experiencing regular episodes of hypoglycaemia require prompt review by the diabetes team.
- Severe episodes of hypoglycaemia require urgent review by the diabetes team.
- To prevent blood glucose levels dropping again, follow sugary foods with 10-20g of a longer-acting carbohydrate such as:
Tell the patient
When you are unwell with any of the following…
- Vomiting or Diarrhoea (unless only minor and mild)
- Fevers, sweats and shaking (unless only minor and mild) – this can often happen with common cold/flu, chest infections, water infections
Then
- STOP taking the medicines I have written down for you
- Restart these when you are well (after 24-48 hours of eating and drinking normally)
- If you are in any doubt, contact the pharmacist, doctor, nurse or call 111.
Also
- Take some rest
- Drink plenty of sugar-free fluids. Aim to drink at least three litres (five pints) a day, UNLESS YOU HAVE HEART FAILURE – in which case ask your Heart Failure nurse or GP or ring 111 (you may need to stick to around 1.5-2 litres). If you have Heart Failure, weigh yourself every day. If you suddenly gain more than 2Kg in 3 days, contact the emergency doctor or call 111.
- Try to keep to your normal meal pattern, but if you are unable to, for any reason, you can replace some or all of your meals with snacks and/or drinks that contain carbohydrate such as yoghurt, milk and other milky drinks, fruit juice or sugary drinks such as Lucozade, ordinary cola or lemonade. You may find it useful to let fizzy drinks go flat to help keep them down
- Avoid too much caffeine as this could make you dehydrated.
- Take painkillers in the recommended doses as necessary.
- Contact your GP to see if treatment with antibiotics is necessary.
- If you are vomiting uncontrollably, contact your GP or call 111
- Keep taking your insulin or diabetes medications even if you are not eating. HOWEVER, stop metformin and blood pressure medication if you are dehydrated.
- Test your blood four or more times a day and night (ie at least eight times in a 24-hour period) and write the results down. If you are not well enough to do this, ask someone to do it for you.
- Test your urine four or more times a day and night (ie at least eight times in a 24-hour period) and write the results down. If you are not well enough to do this, ask someone to do it for you.
- Testing for ketones
- When diabetes is out of control as a result of severe sickness, it can lead to a condition called diabetic ketoacidosis or diabetic coma if you have Type 1 diabetes. The body produces high levels of ketone bodies causing too much acidity in the blood.
- If you have Type 1 diabetes and your blood glucose level is 15 mmol/l or more or you have two per cent or more glucose in your urine, you will also need to test your urine or blood for ketones. They are a sign that your diabetes is seriously out of control. Ketones are especially likely when you are vomiting and can very quickly make you feel even worse. If a ketone test is positive, contact your GP or diabetes care team immediately.
Medicines to STOP on sick days (mnemonic SADMAN)
- SGLT-2 inhibitors: medicine names ending in “flozins” like canagliflozin, empagliflozin, dapagliflozin
- ACE inhibitors: medicine names ending in “pril” like ramipril, lisonopril, enalapril, captopril, perindopril
- Diuretics: e.g. medicine names ending in “ide” like furosemide, bendroflumethiazide, bumetanide
- Metformin (which is a medicine for diabetes)
- ARBs: medicine names ending in “sartan” like losartan, candesartan, valsartan, irbesartan
- NSAIDs: anti-inflammatory pain killers like ibuprofen, diclofenac, naproxen, ketoprofen
Advise patients of the following:
- Vaccinations and/or malaria tablets
- Carry diabetes ID or a GP letter if carrying insulin and list of prescription drugs
- Carry all medication and blood glucose testing equipment in hand luggage
- Consider how to keep insulin cool if travelling for long periods
- Travel insurance: – Allow 2 weeks to buy travel insurance. – Don‟t just buy on price, check the cover and read the small print – – Be honest and declare all medical conditions
- Plan to take twice the quantity of medical supplies normally used
- Consider adjusting medication if travelling across time zones
- Consider adjustment to insulin if travelling to hot or cold climate
- Carry a European Health Insurance Card (EHIC) if travelling within Europe
www.ehic.org.uk, / 0845 605 0707
Consider availability of insulin if travelling abroad for long periods.
Interpreting blood results on pathology template – Remember frailty
- HbA1c <48 →select satisfactory→take no action – patient will be reviewed as per recall
- HbA1c 48-53 →select abnormal →speak to nurse → send task to admin to book tel appt with nurse to discuss abnormal result and document a suggested plan to up-titrate medication based on the above guidance for nurse to discuss with patient – nurse will discuss with patient possible changes to medication and then task Dr back to make changes and issue script. – if on single drug or diet only
- HbA1c <53 → select satisfactory →take no action – if on SU or combination drugs patient will attend at next review 6 months later
- HbA1c >53 → select abnormal (take into account patients age and fraility) →speak to nurse → send task to admin to book tel appt with nurse to discuss abnormal result and document a suggested plan to up-titrate medication based on the above guidance for nurse to discuss with patient – nurse will discuss with patient possible changes to medication and then task Dr back to make changes and issue script.
Any concerns – send message to Level 2 team
Using the SystmOne Template (CDM) for Diabetes.
See CDM review table
- Bloods: U&Es, eGFR, HbA1c, ALT (if first year on statin) and lipid profile – (Consider other tests if have other chronic diseases.)
- Urine ACR.
- BP
- Lifestyle discussion: smoking status/cessation advice, exercise status, alcohol intake, diet.
- BMI
- Retinal review.
- Foot check annually (in house) and record on the template. If moderate or high risk they need a referral to podiatry
- Any complications? erectile dysfunction, neuropathic pain, autonomic neuropathy.
- Hypo unawareness, ? hypos requiring external intervention (see DVLA guidelines).
- Review of blood monitoring – if they require monitoring.
- Medication review: concordance/indications/side effects/if on insulin – injection sites.
- Record medication review done, move date on till next review
- Assign diagnosis to repeat template medication.
- Add/move recall on. NB: Diabetics well be reviewed at least 6 monthly.
TARGETS AT A GLANCE
- BP: <130/80 – particularly if there are renal problems
- Get to non smoking: don’t forget smoking cessation
- Cholesterol: < 4.0mmol/l
- HbA1c:
- Diet alone or single drug not affected by hypoglycaemia <48mmol/l
- Medication <53mmol/l. Patient tailored care needed especially if they are elderly or there are concerns about hypogylcaemia.
- BMI: <25
Diabetes in pregnancy is associated with risks to the woman and the developing fetus.
Planning a pregnancy
Women planning a pregnancy should be referred to a diabetes pre-conception clinic.
Pre-pregnancy planning includes:
- Diet and exercise, weight loss advised if body mass index > 27kg/m2
- Retinal photography unless carried out in last 12months
- Renal assessment (including microalbuminuria)
- Folic acid 5mgs for 3 months preconception and continued for first trimester.
- Establish rubella status, booster organised if required.
- Blood pressure should be monitored
- Smoking/alcohol cessation advice
Review of medications
- Metformin may be used before and during pregnancy, as well as or instead of insulin. The diabetes antenatal clinic will oversee their care whilst pregnant.
- Isophane insulin is the first-choice long-acting insulin during pregnancy.
- Discontinue oral hypoglycaemic agents (apart from metformin), ACE-inhibitors, Angiotensin Receptor Blockers and statins
Gestational diabetes
- 6 weeks post-partum patients require a HbA1c to establish whether glucose tolerance has returned to normal.
- All patients require advice on their elevated long term risk of diabetes.
- All patients require advice on their risk of gestational diabetes in future pregnancies.
- All patients require advice regarding diet, weight control and exercise
All patients require an ANNUAL HbA1c in view of their elevated risk of Type 2 diabetes. Please add an ‘AT RISK OF DIABETES’ recall to their notes.
Ramadan & Fasting Advice for Diabetics
Fasting is an obligation for competent, healthy adult Muslims although there are exemptions. Many of those who could seek exemption might still want to fast. It is important to respect this but it is advisable to start planning 6-8 weeks before Ramadan to avoid adverse outcomes e.g. patient self-adjustment of medication.
The fast of Ramadan lasts from dawn to sunset for a period of 29 or 30 days. It follows the lunar calendar so is brought forward by about 10 days each year. Fasting people generally eat two meals a day: often a smaller meal before dawn (Suhoor) and a larger one after sunset (Iftar). No fluids or food are taken during daylight hours. This includes water and most medication.
Who is exempt from fasting?
- Acute or chronic illness
- Travellers
- Pregnant/breastfeeding*
- Menstruating/postpartum bleeding
- Children
- Mentally unwell/lacks capacity
*Consensus by Islamic scholars that it is permissible not to fast if there is threat of harm to mother/child
Permissible interventions/medications
- Blood tests
- Vaccinations
- Asthma inhalers*
- Ear drops*
- Eye drops
- Transdermal patches
*Difference of opinions exist. Encourage patients to contact their local imam, or BIMA for advice.
The following is a guide summarised from the International Diabetes Federation (IDF)
| Usually taken | During Ramadan |
Metformin | Once daily | With evening meal |
| Twice daily | With evening + dawn meal |
| Three times daily | If well controlled, take lower-than-usual dose at dawn meal Take normal dose with evening meal |
Sulphonylurea | Once daily | With evening meal |
| Twice daily | If well controlled, take lower-than-usual dose with dawn meal Take normal dose with evening meal |
pioglitazone | – | No dose adjustment |
Gliflozins (SGLT2 inhibitors) | – | Use with caution but no dose adjustment needed. Take with evening meal. Increase fluids in non-fasting hours if possible. |
GLP-1s | – | No dose adjustment needed |
Should I advise my patient NOT to fast?
BIMA have an interactive traffic light tool that help to classify patients into low/moderate risk, high risk, and very high risk at
- www.britishima.org/Ramadan-compendium
- in chapter 6.
Patients in the two higher tiers should be advised that they ‘must not fast’ and ‘should not fast’ respectively. Consider advising these patients to fast in the shorter winter months. If they insist to fast, monitor regularly and ask that they should be prepared to break the fast in case of adverse events. Below is a shortened summary of the advice:
MUST NOT FAST
V. HIGH RISK
- Severe hypoglycaemia in last 3 months
- DKA in last 3 months
- Recurrent hypos
- Hypoglycaemia unaware
- Poorly controlled T1DM
- Acute illness
- T2DM on insulin and no experience of safe fast
SHOULD NOT FAST
HIGH RISK
- T2DM sustained poor glycaemic control e.g. HbA1c >75 for 12 months
- Well controlled T1DM
- T2DM on MDI or mixed insulin
INDIVIDUAL DECISION - WHAT IS THEIR ABILITY TO TOLERATE IT - LOW RISK
- Well controlled T2DM

