The full GP Training Roadmap from ST1 to ST3
Which Assessment at Which Stage?
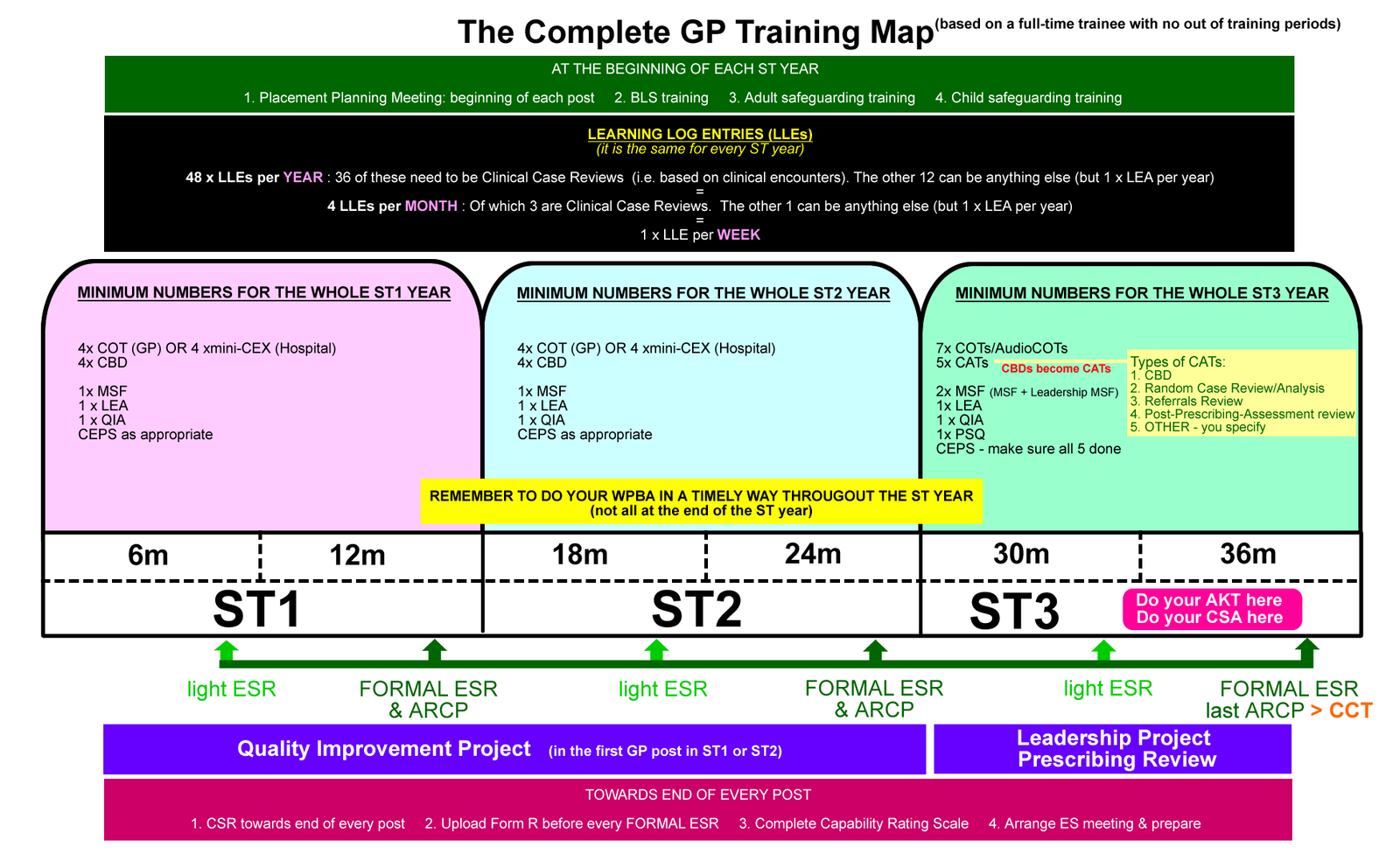
This page outlines the MINIMUM WPBA type assessments (like CBDs, COTs and CEXs) for each ST post. You should aim to do significantly more than the minimum number! And they all need to be done in a timely way (i.e. spread out and not all last minute) before the ARCP panels in June.
YEARLY for the full-timer...
6 MONTHLY it will be...
ST1
every 6 months...
- Log entries (24 minimum = 1 per week; 18 of 24 need to be Clinical Case Reviews)
- CBD x 2 (minimum)
- Mini-CEX or COT x2 (minimum). COT in GP, CEX in hospital.
- CEPS as appropriate
PLUS in the whole ST year
- MSF x1
- LEA x1 (a mild significant event type thing)
- QIA x 1
- QI project x1 (if in a GP post)
ST2
every 6 months...
- Log entries (24 minimum = 1 per week; 18 of 24 need to be Clinical Case Reviews)
- CBD x 2 (minimum)
- Mini-CEX or COT x2 (minimum). COT in GP, CEX in hospital.
- CEPS as appropriate
PLUS in the whole ST year
- MSF x1
- LEA x1 (a mild significant event type thing)
- QIA x 1
- QI project x1 (if in a GP post)
ST3
every 6 months...
- Log entries (24 minimum = 1 per week; 18 of 24 need to be Clinical Case Reviews)
- CATs x 2-3. e.g. CBDs, RCAs, Referrals, Ix review. Minimum 5 by end of ST year.
- COT x 3-4. At least one Audio-COT. Minimum 7 by end of ST year
- CEPS – get all mandatory 5 done by ST3 end
PLUS in the whole ST year
- MSF x 2 (MSF + Leadership MSF)
- LEA x1 (a mild significant event type thing)
- QIA x 1
- Leadership Project x1
- Prescribing Review x1 (60 prescriptions)
- PSQ x1
Other Notes
Trainees are often puzzled as to when to do some of the things like AKT and CSA, amongst other things. It’s understandable because there are so many elements and deadlines to GP training in the UK. So, this page is an attempt to demystify some of that and help you make some decisions for yourself. Many trainees are of the mindset of wanting to get things “out of the way”. This is dangerous territory – some of the things (like the exams) are at quite a financial cost. Wouldn’t you prefer to take them just the once and pass? As for the exams, you need some good experience in General Practice in order to pass them. So, don’t be in a hurry to get everything out of the way. Relax, and enjoy the learning process.
At the very minimum, you should not attempt the AKT until you are in your first post of ST3 in General Practice. Why? Because you can read all you want, but some of the questions will be around specific GP stuff that you might not find in the academic books about General Practice.
In terms of CSA, again it is best to take it in your ST3 – in fact, you can’t take it any earlier. The CSA requires a lot of practise as well as knowledge. You need to practise your consultation, clinical and organisational skills in the first 6m of ST3. Then towards the end of your 1st 6 months of ST3, or at the beginning of the 2nd 6 months, you should be ready to go.
Many GP educators believe that you should take both AKT and CSA roughly at the same time towards the beginning of your 2nd post in ST3. Why? Because both exams require a good level of clinical knowledge, so why not revise to cater for both exams? The CSA is not just about communication skills. So, the knowledge you will have gained from preparing for the AKT will be “fresh” for the CSA too. But also, don’t sit them too late! Whilst we hope you pass them easily, you are strongly advised to sit the AKT and CSA early enough in ST3 to allow yourself sufficient time to resit before the end of 34 months of training. So, about the beginning of your 2nd 6 months of ST3 should be about right for most of you.
We’ll let you decide which you think would be best for you. Have a chat with your trainer.
- You are responsible for knowing and organising which assessments need to be completed in each post and organise them. You decide when these assessments take place. Therefore, you (the trainee) need to tell your trainer or hospital consultant when you are ready to do a specific type of assessment (not the other way around). When you qualify, you will have to engage in annual GP appraisal where you gather evidence of your performance. No one will be there to hold your hand or remind you. So, it’s important to develop this persona of the responsible self now. Your trainer may not remind you, partly because they will be monitoring or assessing your engagement with self-responsbility.
- Give your trainer/hospital consultant adequate notice (“Can we do a CBD next week?”). Pace yourself; your trainer or hospital consultant won’t be happy if you try and squeeze all the assessments into the last few weeks of your post.
- Help your hospital consultants out. Some of your hospital colleagues may not be that familiar with what they are doing in the GP assessments. They are hospital specialists in their particular field, and it is understandable that they would be confused or not so clear about some of the things we require from a GP point of view. So, please help them by firstly, attaining a good understanding of how the assessments work and what each domain or competency means so that (secondly) you are empowered to help guide your consultant if they are struggling or confused with something. In this way, we are sure that your hospital consultants will get the hang of our GP training things in no time and in return it will really help you to get the best out of them. So, please help them.
- Please do not see ‘needs further development’ as a failure. In fact, it is THE EXPECTED GRADE for many of you in ST1 and St2. We expect you to have quite a few ‘needs further development’. If you had all “competent” or “excellent” grades in ST1 or ST2, we’d be worried – how can you have no learning needs at such an early stage in your training?
- Complete the minimum number of assessments before at least 1 month BEFORE the end of your post. They need to all in place before your Educational Supervision meeting. Otherwise, the Educational Supervisor cannot sign you off. Remember, the minimum number of assessments IS THE MINIMUM NUMBER. You should be aiming to do lots more.
Do you feel confused and overwhelmed by all the different WPBA things that you ahve to do? Your confusion is understandable. It took us GP Trainers and TPDs a while to get used to them too. So, be reassured that being confused and overwhelmed by what you need to do and by when is normal for most trainees. Here are some quick points about some of the assessments.
- Remember again that MINIMUM numbers are MINIMUM – you should be aiming to do a lot more!
- Write about one log entry per week. Use “Ram’s easy way to write learning logs”
- Just to re-emphasise the point about the number of learning log entries. Basically you need to do 36 Case Review type of Learning Logs every year (previously called Clinical Encounters), This equates to 3 per month or about 1 a week. But you still need to write logs about other things like learning from HDR, reading, reflections on the post etc. However, you can’t include them in the 36 figure because they are not Case Reviews. Case Reviews are essentially learning from your clinical encounters with patients at your place of work. Personally, I think they should have stuck with the term Clinical Encounters because the term is self-explanatory!
- Significant Event Analysis – no official numbers. Just do them as and when appropriate/relevant.
- CBDs & COTs – preparation is necessary. Don’t just do them last minute because case selection is very important. Different cases will allow demonstration of different Professional Capabilities, and you need to cover all of them to complete GP training.
- Mini-CEXs are done in hospital posts and not in GP posts. In GP posts, you do COTs instead.
- CEPS – try and get many of these done during your hospital post.
- PSQs will only be assessed in the primary care setting.
- MSF will involve clinical raters only when in secondary care BUT both clinical and non-clinical raters (e.g. admin team) when in primary care.
- CSR does not need to be completed if the CS is the trainee’s ES. This often applies to first placements in GP during ST1 or ST2.
- The Mid-Year Review is essentially a light-touch ES meeting where everything in your eP is reviewed to ensure you are on track for training. However, no ESR needs to be generated but ask your ES to write a summary of Good Points, Not So Good Points & Things to Work On as an Educator’s Note.
- Remember, everything should be in order by the 34 month stage of GP training. The last 2 months should be reserved for your ES and ARCP panel meetings to make their final judgements about you.


Thanks for giving time and efforts in posting this valuable information.
Thank you so much for this. Very helpful