Gastroenterology
Bradford VTS Clinical Resources
- by Dr Sabah Malik
- Last modified: 30th April 2024
- No Comments
DOWNLOADS
path: GASTROENTEROLOGY
WEBLINKS
……………………………………..
Information provided on this medical website is intended for educational purposes only and may contain errors or inaccuracies. We do not assume responsibility for any actions taken based on the information presented here. Users are strongly advised to consult reliable medical sources and healthcare professionals for accurate and personalised guidance – especially with protocols, guidelines and doses.
COME AND WORK WITH ME… If you’d like to contribute or enhance this resource, simply send an email to rameshmehay@googlemail.co.uk. We welcome collaboration to improve GP training on the UK’s leading website, Bradford VTS. If you’re interested in a more active role with www.bradfordvts.co.uk (and get your name published), please feel free to reach out. We love hearing from people who want to give.
……………………………………..
Bowel Cancer
d
c
xxx
Lower GI Fast track referral and FIT, NICE August 2023
Direct 2WW referral | FIT before referral | |||
| Any age | >40 | >50 | >60 |
|
|
|
| |
FIT >10 2ww No fit result or fit < 10: either safety net OR can still refer 2ww if strong suspicion | ||||
xx
xx
Raised ALT & MASLD (Fatty Liver Disease)
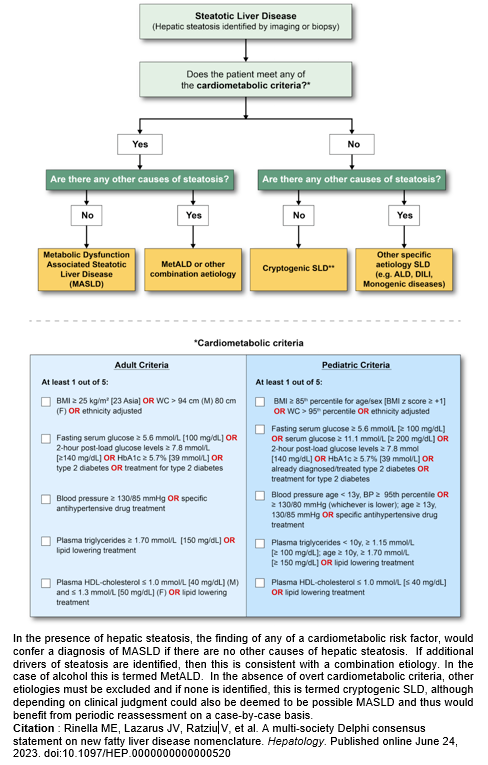
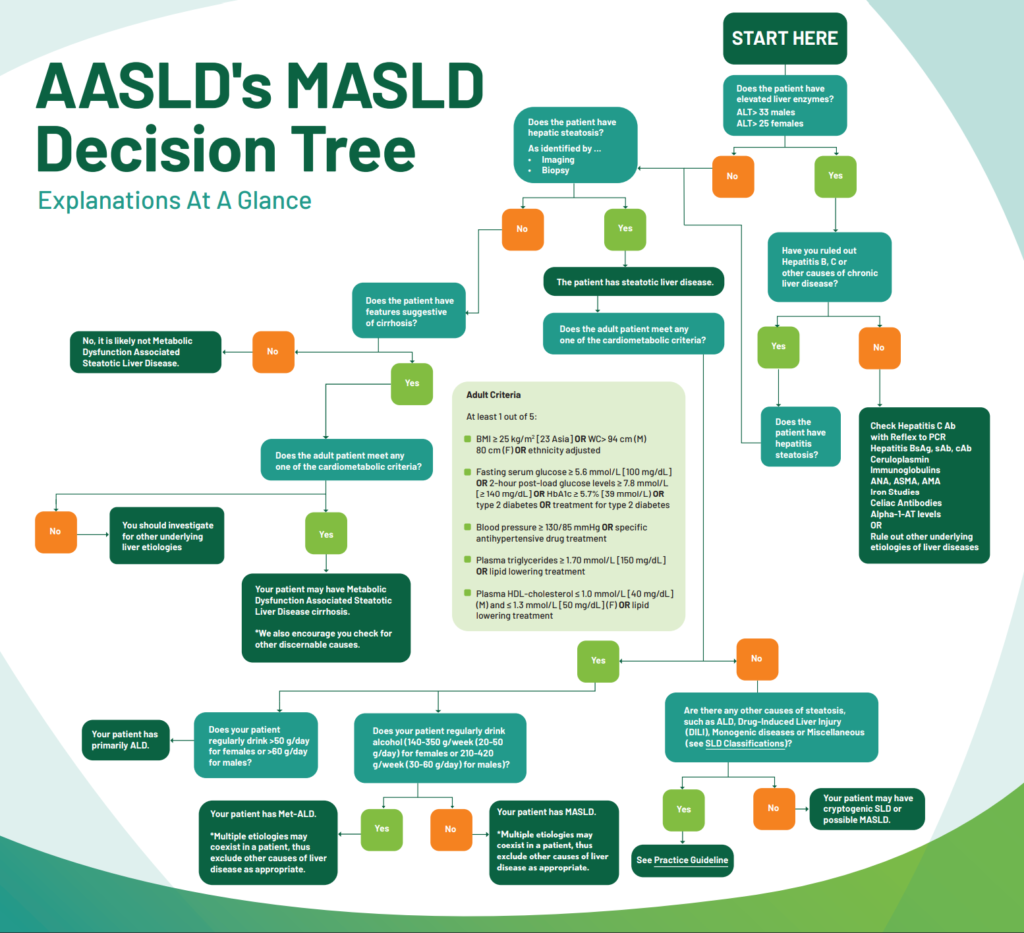
New terminology.
- NAFLD is now called MASLD (pronounced MAA-zuld).
- NAFLD = Non Alcoholic Fatty Liver Disease
- MASLD = Metabolic dysfunction Associated Steatotic Liver Disease
- Steatotic means “fatty”
So why the change?
In the late 2010s, NAFLD, posed a significant threat, sometimes leading to liver failure and the need for expensive transplants. The name “fatty liver” was scientifically inaccurate and the words “fatty” and “alcoholic” made patients feel uncomfortable and doctors to consider it trivial. Renaming it was hoped to lead to a better understanding of the disease. As this stealthy liver disease becomes more common, the search for treatments intensifies, and it is now taken more seriously. Around 25% of adults have MASLD, and of those, about 20% having a more severe form marked by liver scarring and inflammation. The reclassification didn’t stop at MASLD; a new category, MetALD (metabolic dysfunction associated and alcohol associated liver disease), was introduced for patients with MASLD who consume over 210 grams of alcohol weekly. The aim was to clarify what the disease was rather than what it wasn’t, as the old nomenclature didn’t accurately represent the underlying pathology. This change presents an opportunity to raise awareness about liver health in both adults and children.
Interestingly…
Disease names have historically changed for various reasons. For instance,
- Wegener’s granulomatosis became granulomatosis with polyangiitis due to Wegener’s ties with Nazism.
- Primary biliary cirrhosis became primary biliary cholangitis as not all patients had permanent scarring at diagnosis.
- Prejudices have influenced sickness names historically;
- HIV/AIDS were initially called gay-related immune deficiency – renamed with emerging information and better understanding.
- In the 14th century, syphilis had different names based on regions and enemies. The French called it “Neapolitan disease,” the Italians “the French disease,” the Russians dubbed it “the Polish disease” and the Polish named it after Germans! Quite funny when you think about it.
Oh, and the time it takes to change a disease name can be 20+ years!
MASLD is only one type of steatotic liver disease. But it is the most commonest cause!

Source: https://www.aasld.org/new-masld-nomenclature
If MASLD likely (e.g. overweight) – do blood screen and USS
If MASLD unlikely
- consider cause e.g. new medication, illness or alcohol
- Repeat LFTs ~3w later.
- If still raised bloods/USS as below.
ALT < 3 upper limit normal |
| If fatty liver disease = annual recall for bloods. |
ALT 3-5x upper normal limit |
| |
If ALT > 5 x upper limit normal |
| |
INVESTIGATIONS | BLOODS & LIVER USS FBC, U&E, HbA1C, Lipid Screen, LFT (look at AST), TFTs, Ferritin plus…
| |
For Clinician/Nurse/HCA to do
- Work out NAFLD fibrosis score (Fib 4): https://www.mdcalc.com/calc/2200/fibrosis-4-fib-4-index-liver-fibrosis. This will tell you who needs referral to hepatology. Also, refer to hepatology if ALT raised over x3 upper limit normal
- Give information about Fatty Liver Disease: https://patient.info/healthy-living/alcohol-and-liver-disease/non-alcoholic-fatty-liver-disease
- Give lifestyle advice – especially around alcohol and BMI. https://mylivingwell.co.uk/
- Set a recall for every 12 months to do the following (should be a template in your clinical system)…
- Alcohol intake, smoking, weight, BP
- Signpost to Living Well website again: https://mylivingwell.co.uk/
- Annual Bloods: FBC, U&E, LFT (including AST), Hba1c (unless having hba1c for diabetes recall), Lipid screen
https://www.mdcalc.com/calc/2200/fibrosis-4-fib-4-index-liver-fibrosis
This will tell you who needs a referral to hepatology.
e.g through Patches, AccuRx or SystmOne Communications Annexe etc
First SMS Message (before USS done)
Your liver test is abnormal. You need some further blood tests- please contact reception for an appointment and I have arranged an ultrasound scan for you (you will get a letter).
It is important your weight is in a healthy range. If you want help, please see https://mylivingwell.co.uk/
We can discuss this further once we have all the results – usually takes 2 weeks, so book a routine appoint with GP at the 3-4 week stage.
Second SMS Message (after USS done which shows Fatty liver only)
Your liver test is abnormal. Your ultrasound showed you have Fatty Liver Disease. Please read this link to understand it more: https://patient.info/healthy-living/alcohol-and-liver-disease/non-alcoholic-fatty-liver-disease
It is extremely important you ensure your weight is in the normal range and you do not exceed 14 units/alcohol/week. If you would like to discuss this further, please book an appointment with a practice nurse.
We will repeat your liver tests every year to ensure it is stable.
Ramadan & Fasting Advice for Gastro Disease
Fasting is an obligation for competent, healthy adult Muslims although there are exemptions. Many of those who could seek exemption might still want to fast. It is important to respect this but it is advisable to start planning 6-8 weeks before Ramadan to avoid adverse outcomes e.g. patient self-adjustment of medication.
The fast of Ramadan lasts from dawn to sunset for a period of 29 or 30 days. It follows the lunar calendar so is brought forward by about 10 days each year. Fasting people generally eat two meals a day: often a smaller meal before dawn (Suhoor) and a larger one after sunset (Iftar). No fluids or food are taken during daylight hours. This includes water and most medication.
Who is exempt from fasting?
- Acute or chronic illness
- Travellers
- Pregnant/breastfeeding*
- Menstruating/postpartum bleeding
- Children
- Mentally unwell/lacks capacity
*Consensus by Islamic scholars that it is permissible not to fast if there is threat of harm to mother/child
Permissible interventions/medications
- Blood tests
- Vaccinations
- Asthma inhalers*
- Ear drops*
- Eye drops
- Transdermal patches
*Difference of opinions exist. Encourage patients to contact their local imam, or BIMA for advice.
Should I advise my patient NOT to fast?
BIMA have an interactive traffic light tool that help to classify patients into low/moderate risk, high risk, and very high risk at
- www.britishima.org/Ramadan-compendium
- in chapter 6.
Patients in the two higher tiers should be advised that they ‘must not fast’ and ‘should not fast’ respectively. Consider advising these patients to fast in the shorter winter months. If they insist to fast, monitor regularly and ask that they should be prepared to break the fast in case of adverse events. Below is a shortened summary of the advice:
MUST NOT FAST
V. HIGH RISK
- Established cirrhosis
- Active IBD
- Significant acute or chronic diarrhoea
- High output ileostomy
SHOULD NOT FAST
HIGH RISK
Liver transplant on tacrolimus
(high risk renal toxicity if dehydrated)
INDIVIDUAL DECISION - WHAT IS THEIR ABILITY TO TOLERATE IT - LOW RISK
- Low mortality risk cirrhosis (i.e Child-Pugh score class A)
- Stable IBD
- Peptic ulcer disease
- IBS

