Your GP Post Timetable
THE WORKING WEEK TIMETABLE
WEBLINKS
- Doctors & the European Working Time Directive (EWTD) by BMA
- New GP Trainee Working Week Contract as per Junior Doctors’ Committee 2016 (EXCELLENT)
Induction Toolkit
to help GP Trainers
GP Training Map
an 'at a glance' summary
Desktop Consultion Dashboard
for use in the GP consultation
Community Placements
advice and tips
What can a trainee expect from a GP post?
Here is a graphical representation of what you can expect from your training practice. Please remember that all GP training practices work differently. This means that different practices will:
- have varying numbers of partners, salaried doctors, nurses, admin and other staff.
- operate different appointment systems – some may run at 2h, 2.5h or 3h surgeries.
- vary in the way they use computer technology.
- differ in the average number of home visits they do.
- vary in the types of patients they see and other demographics.
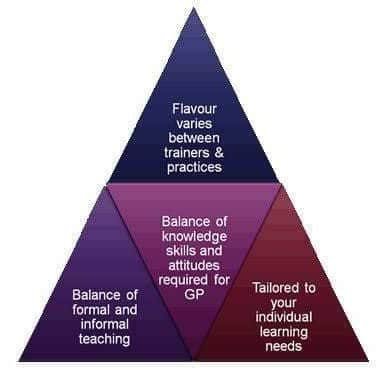
What this ultimately means is that GP trainees in different practices will be exposed to different types of work and varying amounts of workload. In order to protect the trainee from being overworked, a good benchmark is that trainees should not be doing more than what the average doctor at that practice is doing. The scheme expects the trainee to engage in whatever is normal for other doctors at that training practice – despite whatever might be happening at another practice. Trainees should not be comparing themselves and complaining about a ‘lighter load’ in a different practice (unless they really think that the training practice is treating them unfairly). If this is the case, one should discuss it with the GP trainer and the Practice Manager in the first instance before contacting the Training Programme Director.
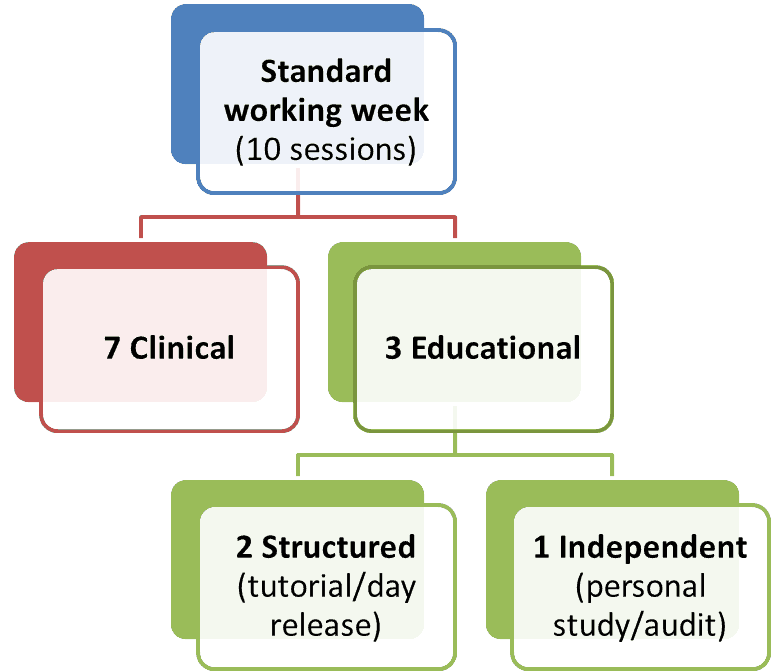
The GP Trainee's Working Week - guidelines
- The standard GP trainee working week consists of 10 sessions. These will be divided into 7 clinical sessions, and 3 educational sessions..
- This structure formalises protected educational time for the trainee and their trainer and thus provides a clear definition of the standard GP trainee working week.
- It provides an excellent practical mix of clinical and educational sessions. A session is defined as 4 hours.
- The structure is also a good basis from which part-time/flexible trainees can work out their weekly schedule.
- The pattern of work will be different in each practice but the overall number of hours should be the same.
- Flexibility is required when implementing this approach i.e. an extra educational session may be substituted for a clinical session to meet specific training needs or to help the struggling trainee with additional needs.
- Educational Sessions are also 4 hours but they can be split up across the week e.g. half-hour debriefs can be added together to make up educational time and personal study can be split into smaller blocks across the week.
- Structured educational time in practice can include tutorials, debriefs, clinical meetings, protected learning time sessions and joint surgeries but not OOH sessions.
- Joint surgeries are considered educational time if clinical workload is reduced by 50% e.g. 20 minute appointments instead of 10 minutes.
- Many trainers prefer having split tutorial times that one big lump sum. Remember, the trainer and trainee cannot concentrate for a full 3 hours; hence most prefer 2 sessions per week of 1.5 h duration.
- It is important to ensure the GP trainee undertakes at least one independent educational session per week due to the intensive training nature of the GP trainee year. This should be timetabled in as a ‘personal study’ session of 4 hours duration. However, this does not mean that there is an “automatic” right to a half day as this will depend on individual practices timetables. The independent educational session should be for personal study, ePortfolio work, audit, WPBA preparation and other admin work.
- On days where there is no Half-Day Release (HDR) session, this does not become an automatic day off. Trainees are expected to inform their practices that there is no HDR session. Instead, trainees should return to the GP surgery to work.
- Sessions can be spread across the period of the post e.g. a longer course involving a whole or several days will result in less clinical sessions that week which can be “paid back” on weeks when there is no VTS session. This does not apply to induction.
- All surgeries must be followed by a debrief. This must be scheduled in and clearly visible on the trainee’s timetable. Debriefs should be 20 mins for a 2 hour surgery and 30 minutes for anything longer.
- Clinical Supervision: GP trainees must be supervised at all times. In other words, someone has to be available for giving advice (and be available on site). This cannot be a locum GP. It has to be a GP partner or regular salaried GP. Someone should be available even when a trainee engages in baby clinic or child immunisations with the practice nurse. It must be clear from the timetable WHO is the Clinical Supervisor for that day.
REST PROVISIONS
- Trainees should only work 40h per week MAXIMUM
- OOH is in addition to this 40 hour working week even at EWTD 2009 (48 hours/week) this will be compliant.
- However time off the following day may be required.
- There must be…
- 11h continuous rest in every 24h
- Minimum 20min break if shift > 6h
- Minimum 24h rest every 7 days or minimum 48h rest every 14 days
- Maximum 8h work in every 24h for night workers
Is the GP Trainer being protected?
- For those who belong to the Yorkshire & Humber GP School, the Trainer’s timetable should also include a 1 hour weekly GP training admin time for each trainee they have.
- This is to enable the GP trainer to perform the administrative duties of being a GP Trainer (like reading ePortfolio entries, following up on projects, reading reports and comments from others etc).
- If you belong to another GP School or Deanery – check if they have a similar stance. If not, suggest it to them. It is good practice as it is imperative that vital activities like GP training are not rushed or squeezed in. There is a need for protected time.
Practice Managers: some considerations when constructing a timetable
Every timetable must be tailored to the individual trainee. Do not just impost a generic one that you have used for GP trainees before. By all means use a generic one that you have used before as a starting point but then tweak it based on the following….
- The number of sessions: are they full-time or part-time?
- Part timers: try to ensure as much overlap as possible between the trainer and the trainee (at least 50%). Get them to work days the trainer works.
- Make adjustments to the timetable for any particular trainee needs.
- For example, surgeries might start later or finish earlier if there are child care issues.
- If a trainee is struggling or has acute social/home issues, at my training practice, we would temporarily put in some appointment blocks to make surgeries feel less pressured.
- If the trainee needs to be away on certain days (e.g. academic GP trainee), provide for that.
- Don’t forget the mandatory things that need to be clearly visible on the timetable
- Who the daily Clinical Supervisor is
- Protected debriefs after each surgery and by whom?
- Half Day Release slot
- Admin slot
- Personal Educational Time Slot
- When you make any of these adjustments, please finally check them through with the GP trainer. The GP Trainer must approve these fine adjustments.
- When the trainee is nearing their AKT exam, remind the trainer if they want to focus the tutorials on increasing knowledge levels.
- When the trainee is nearing the CSA (perhaps 4 months before), ask the trainers if they wish to focus the CSA on role-playing scenarios with a combination of “sit and swap” surgeries.
- And finally, make sure the weekly hours do NOT exceed 40h.
Appointment Length
The following is based on a full-timer GP trainee (who will be with you for 6 months [=24 weeks]). In summary, an ST1 will usually start on 30 min appointments and we gradually work them down to 15 minute appoints. An ST3 will usually start on 30 min appointments and we gradually work them down to 10 minute appointments. Moving the appointment time down in a graduated way is important so that they get adequate clinical exposure to help them acquire a breadth of clinical knowledge and skills that is necessary for passing their professional exams like the AKT and CSA.
- ST1 or ST2 no previous FY placement in GP
- First 2w: no surgeries – sitting in
- Next 4w: 30 min appointment per patient
- Next 10w: 20 min appointment per patient
- Final 8w: 15 min appointment per patient
- ST1 or ST2 WITH previous FY placement in GP
- First 2w: no surgeries – sitting in
- Next 2w: 30 min appointment per patient
- Next 12w: 20 min appointment per patient
- Final 8w: 15 min appointment per patient
- ST3-1
- First 2w: no surgeries – sitting in
- Next 1w: 30 min appointment per patient
- Next 5w: 20 min appointment per patient
- Next 12w: 15 min appointment per patient
- Final 4w: 10 min appointment per patient
- ST3-2 continuing from ST3-1
- For the last 6 months : 10 min appointment per patient
- ST3-2 transfer from another practice
- First 1w: no surgeries – sitting in
- Next 1w: 20 min appointment per patient
- Next 4w: 15 min appointment per patient
- Final 18w: 10 min appointment per patient
- ST1 or ST2 no previous FY placement in GP
This 30-20-15 minute model allows the trainee to gradually adapt from hospital medicine (where they’ve usually spent an hour or so taking a history and examination) to the general practice model of 10 minutes. It also gives them time to get used to the new computer medical system. Some move steadily at the usual rate but others will need more time.
The Weekly Tutorial (and WPBA assessment slots)
- All GP trainees must be slotted in for a 3 hour weekly tutorial. The way you do this is up to you.
- 3 hours all in one go is probably a bit too much and perhaps two lots of 1.5 hour tutorials across the week (followed by a shortened surgery) would educationally fair better.
- What you cover in these tutorials is up to you. You might want to cover some clinical topics, significant events, problem cases, random cases, or something else. However, you must also reserve some of these slots for the mandatory MRCGP assessments that you are expected to carry out – namely, Case Based Discussions (CBDs) and Consultation Observation Tools (COTs).
- There is a MINIMUM number of each of these WPBAs that need to be done – but please remember that these are MINIMUMS and you should be aiming to do a lot more. If this minimum number is not achieved, a trainee can be asked to repeat an ST year – in other words, the consequences are big!
- In my practice the way I ensure that these assessments happen in an effortless way is to schedule a Monday 1.5h tutorial dedicated to doing COTs and a Weds 1.5h tutorial dedicated to doing CBDs. That doesn’t mean I always do COTs on a Monday and CBDs on a Weds – it’s just there to mark their default position. We might occasionally veer off and do a Random Case Analysis, another CAT or a review of significant events and sometimes even a clinical topic. I probably stick to doing a COT and CBD on their allocated days around 60-70% of the time. In this way, I don’t have to count numbers – I know we will end up doing lots more than the stipulated minimums.
- Remember: in a 6 month period, there are 24 weeks, but perhaps only 18 available for tutorial as 6 weeks will be hijacked by annual leave – theirs or yours. So, make the most of it.
Scheduling weekly video surgeries into the timetable
It is important for the Practice Manager to ensure that the GP trainee’s weekly timetable includes a surgery where the trainee records his or her consultations with patients. The material for this will then form the basis of either COT assessments or tutorials around communication skills in the following week. The once a week video session will help the GP trainer build on what has gone before. The weekly video session is non-negotiable and the Practice Manager will need to observe the following when slotting it into the GP trainee’s weekly timetable.
- The recorded video surgery will happen ONCE a week in the GP trainee’s timetable. It will be clearly marked on the timetable. In fact, if there is a choice – ask the trainee which days they would like to do the video on.
- The video surgery will be in place after month 1 of the trainee being in the practice.
- The video surgery will last a maximum of 2.5 hours and patients booked at 20 minute slots. Make sure that it is clearly visible on the computer’s appointment system that this is a video surgery.
- A regular day is better than different days otherwise it becomes organisationally difficult to do and remember for all staff concerned.
- The Practice Manager can delegate this role to Admin staff.
- There must be a clear process of gaining consent from the patient that is initiated by a member of the reception team. They must be trained and versed in obtaining consent in an patient-orientated ethical way that easily makes it okay for the patient to say no. Use the COT consent form. A signature must be collected before and after the consultation. The second signature confirms whether the patient is happy or not – after all, how can a patient truly consent to their consultation being shown to someone else when they have not yet been through it? The second signature is important.
- There must be a clear system of storing the consent forms which can be discarded after 1 year.
- The patient must be made aware: how long the video will be kept for (usually under 6 months), that it will only be used for training purposes and reassurance that it will be deleted after this time.
- Make sure the new GP trainee understands the protocol for video surgeries. It would be good to have a written practice document summarising the process.
- The Practice Manager, the GP trainer and the GP trainee must make themselves familiar with the Ethical guidelines for recording patients on video document.
Video Allergy
Sometimes, GP trainees can be very apprehensive about doing video surgeries and many don’t like the idea of doing them. It’s not surprising as for many of them it is a new experience. During these sessions, don’t forget that the GP trainer is also analysing their day-to-day performance behaviour – how would you feel if you were in the same position as them? Therefore, it’s important for you to show some empathy and acknowledgement in this regard. So, to help them settle in, reassure them that their feelings are normal and widespread among new GP trainees. Explore their anxieties and fears – try and alleviate them. Emphasise the formative nature of the feedback and the supportive climate in which this will be given. It might be worth you (the GP Trainer) showing a (non-perfect) video of yourself and analysing that – emphasising how no one is perfect and that even you can be taught a thing or two.
Click here to read more about : video allergy — overcoming it (TEACHING RESOURCE).doc
Sit and Swap Surgeries
- Sit and Swap surgeries is where the GP Trainer and trainee take it in turns to see patients. It is one of the best ways of helping trainees acquire communication skills. The GP trainer demonstrates and role models consultation behaviour. Then the trainee has a go at some of the skills. The trainer fine tunes, and the GP trainee continues to “have another go”.
- The Practice Manager needs to schedule regular Sit and Swap surgeries – at least one per month THROUGHOUT THE ENTIRE TRAINING PERIOD. The preferred is 2 per month. Patients need to be booked in at 20 minute intervals. Just book them into one surgery – perhaps under the trainee’s name – otherwise the patient will expect to be consulted by the GP trainer. And then let the Trainer and trainee decide how they want to split seeing them.
- Sit and Swap surgeries should be provided for trainees at all stages, not just ST1s. ST3s have consultation learning needs too – no matter how good they are.
- Trainer – remember that some COTs can be carried out on directly observed consultations (no more than one in any one surgery).
On Call Surgeries
ST1 & ST2 (Beginners)
The ST1/ST2 trainee should not be engaging in on-call alone during the first 6 months of GP training. They have volumes to learn. And we strongly feel that putting them in a clinic where there are high stakes in terms of clinical risk is unnecessary danger for both patients and ST1s and ST2s. In fact, many practices don’t allocate any on-call duty sessions to trainees in their ST1 year because they simply have too much to contend with. Of course, this does not mean that they cannot do any on-call – as long as they are DIRECTLY SUPERVISED, then they can. For example, say from month 3 or 4 onwards, perhaps the a qualified GP can do the on-call but every other patient is seen by the GP trainee whilst they are DIRECTLY supervised in real time by that qualified GP (has to be salaried GP or partner, not a locum).
ST3s (Final Year GP Trainees)
- ST3s need to start learning how to do on-call. After all, they will be doing it when they are qualified. We suggest the following schedule.
- First 3 months: let them settle in, no on-call duties.
- Second 3 months: let them do on-call but you have to directly supervise them in real-time initially. When you are comfortable, move to a method where you both work off the same on-call list but you see the GP trainee and their patient after they have finished so you can check what they have done is okay before the patient leaves.
- Final 6 months: gradually move away from direct supervision towards independent practice as you gain faith in the trainee’s clinical ability. Of course, debriefing along the way.
Please remember, although we have provided you a time schedule above, it is not this alone which should determine how strongly you should supervise the trainee. Whether you go in deep with every patient or have a more light touch approach really depends on your faith in their clinical abilities. This “clinical faith” is determine not only by your continued observation of them, but from multiple sources of feedback like from colleagues, staff, COTs, CBDs, post surgery debriefs and so on. So, how you actually decide really depends on the rate of progression of your trainee and your faith in their clinical abilities. Clearly, they need to be comfortable at doing it well in advance of the completion date for their GP training.
Telephone/Video Consultations
These days, GPs are doing more and more TECHNOLOGY ENHANCED CONSULTATIONS. For example, there are
- e-mail consultations (often called e-Consults)
- video to video consultations (using software like AccuRx)
- Telephone consultation
ST1/ST2
All of these different methods of consulting requires its own set of skills which take a while to develop. We feel it is too much for the GP trainee in the ST1/ST2 year to be learning this when actually what they should be focusing on is basic face-to-face communication skills. Of course, there is not harm in doing the odd “other type” of consultation, but these consultations must not detract from the bread and butter of General Practice which is face-to-face consultations. It would be unfair to throw them at the deep end and get them to cope with telephone/video/email consultations too. Remember, skills need to be build layer upon layer – in a gradual and incremental way. So, for the ST1/2, we would suggest doing lots of face-to-face consultations with just a few eConsults, video-to-video consultations and a few telephone consultations along the way; of course, teaching communication skills along the way.
ST3
For the ST3, it is a different matter. They will have had lots of face-to-face communication skills training that it will be time for them to learn skills for other ways of consulting. This is probably best done in the ST3-2 year. So, in the ST3-1 year (i.e. first 6m of ST3), consider an “introduction” to these different types of session by plugging them into their timetable just here and there with the necessary training from other GPs. But in ST3-2 (the second 6m of ST3) get them to do them more regularly with a mixture of observed and independent practice.
A note for Practice Manager: when you do put them down for these other types of consultations: PLEASE tell both the GP Trainer and the trainee. Other than being courteous and good practice, it will serve as a signpost to the GP Trainer to provide the necessary training to help acquire the appropriate skill set.
Signing prescriptions
Trainees may sign repeat prescriptions as soon as they start general practice. Again, it’s probably best they start doing this only after a period of adequately settling in.
Perhaps from month 2 onwards. The GP Trainer and trainee should engage in a tutorial about repeat prescribing and what’s involved in a medication review prior to this.
Do you have GPs who moan about the time for GP Training?
This is not an uncommon occurrence. At some point in nearly every GP training practice, one or two other GPs who are not trainers sometimes become resentful and angry towards the requirements of GP training. They often feel that they are doing the work and the GP trainer is not. Their minds start doing what minds are naturally good at doing – which is to make unreal conclusions like “it must be lovely sitting back and doing a cosey tutorial over coffee”. They end up moaning about the proportion of time the GP Trainer actually spends on seeing patients (because of “all this protected training time”). But they some how forget what the practice gets in return for 1-2 sessions of the GP trainers time – namely a GP trainee pair of hands that work way more than 2 sessions a week!
So, if you sense any of this, don’t ignore it. Raise the issue and discuss it at a practice meeting. Remember to be kind and compassionate – they are more likely to listen to you and “tell themselves” how they have oversimplified the situation. Please calm down any anger vibes you have because you dont want to add fuel to the fire. Discuss it when you feel okay inside.
Why Do We Do GP Training? (especially as it is not very well paid) These are some of the reasons:
- approval as a training practice is one indication of high standards of record keeping, organisation, premises and patient care
- contact with young doctors is stimulating and keeps everyone more in touch with developments in general practice
- educational activity is a good balance to clinical activity, for both the trainer and the practice; develop your teaching skills
- being a training practice is very valuable for GP recruitment, either directly if an ex-GPR comes to work at the practice, or indirectly because the practice is known via the VTS, or even because potential recruits from outside the area are attracted by a practice’s training status
- you get a free pair of hands (sometimes questionable) and some training money in return
Remind Them…
- Remind them (especially if you’re a part-time GP with a full time trainee) how you are actually seeing more patients with combined forces than if you were operating alone.
- Remind them of the extra pair of hands to do home visits or help out on a particularly busy day.
- Remind them of the liveliness and joy trainees bring to the practice.
- Re-evaluate and re-establish your practice’s ethos towards training by gently re-engaging them (rather than being aggressively passionate).
It’s also worthwhile trying hard to get the practice to see GP training as a practice activity rather than a Trainer-only activity. To do this requires engaging them and getting them to do some of the pleasurable things in GP training like doing clinical tutorials, debriefing trainees, clinically supervising them and so on. In this way, they too will feel the energy and dynamism that trainees bring to one’s working life. Also, try and put a training item or update onto the agenda at most practice meetings (even if it is just for information giving). Try and get discussions going and thereby making the rest of your team feel a core part of GP training. And finally, try and get your Practice Manager to share the same passion as you have for GP training. If anyone can make something happen smoothly – it’s the Practice Manager!
Out of Hours and timetabling adjustments
GP trainees need to engage in Out of Hours (OOH) sessions. They don’t have to do a set or minimum number. But they have to collect enough evidence of exposure and experience in unscheduled urgent care. That experience can come from a number of sources, not just Out of Hours- for instance, the on-call doctor, sessions at the local GP A&E centre, a session with paramedics, sessions with the mental health crisis team and so on.
However, the Practice Manager will need to adjust the timetable in light of these Out of Hours sessions. A GP trainee can only work a maximum of 40 hours per week and that includes this urgent sessions. So, make sure you tell the GP trainee to tell you at the beginning of each week if there are any OOH sessions planned, so that adjustments can be made to the remainder of that timetable that week. Yes, the adjustments need to be made to the timetable for the same week they are doing the OOH session in and cannot be “made up later” in subsequent weeks. In fact, tell your GP trainee to inform you of the sessions as soon as they know – at the time they plug them into their diary – the sooner, the easier it will be to make the necessary timetable adjustments.
REST PROVISIONS
- Trainees should only work 40h per week MAXIMUM
- OOH is in addition to this 40 hour working week even at EWTD 2009 (48 hours/week) this will be compliant.
- However time off the following day may be required.
- There must be…
- 11h continuous rest in every 24h
- Minimum 20min break if shift > 6h
- Minimum 24h rest every 7 days or minimum 48h rest every 14 days
- Maximum 8h work in every 24h for night workers
A quick IMPORTANT note for New Trainers & their Practice Managers
Make sure your timetable incorporates all the rules mentioned above. When it comes to the trainer’s interview – the interviewing panel will want to see the timetable and they will want to see that you have allocated protected time for debriefs, tutorials, personal study time and so on. They will want to see the hours to make sure you are not breaking the 40 hour weekly limit. They will want to know how you will make sure the EWTD is obeyed – for example, when the trainee works an OOH session. They will want to see not just on paper but get a feel that you have it all sorted at a practical functional level.

Hi, This guide is excellent and thank you for making all your resources freely available!
I just wanted to ask about your example GPST timetable (I think I looked at the ST2 one – I couldn’t help but notice that this timetable amounts to a 45.5 hour week, and there are some days where the trainee has just 15 minutes for lunch. As this is an example used by lots of VTSs I wondered if this was definitely correct?