MRCGP & GP Training
Work Place Based Asessment (WPBA)
SPECIFIC PAGES
- MRCGP intro
- Which Assessments & When?
- CBD
- COT
- Audio-COT
- CATs – other consultation tools
- CATs – random case analysis & reviews
- CATs – prescribing review
- CATs – review of investigations
- CATs – referrals analysis
- CATs – debriefs
- CATs – leadership activity/project
- CEXs
- CEPS
- MSF
- PSQ
- NOE
- Community Placements in ST1
- Quality Improvement Project (QIP)
- Leadership Project
- Learning Event Analysis (LEA)
- Significant Event Analysis (SEA)
- The CSR
What is Work-Place Based Assessment (WPBA)?
WPBA assessment is basically a set of assessments that test what you actually do in General Practice. Of course, there are lots of different things we do in General Practice and one of the reasons why there are so many different assessments is to cover the range of things we do (for example, COTs for consultation skills, Audio COT for telephone consultation skills). But the other reason why there are so many different WPBA assessment types is because some of them test the SAME thing – which is a good thing – because it makes assessment more reliable at providing a true picture of you through something called triangulation. Triangulation is is a process by which a teacher collects evidence about how good a student is at something – this evidence is collected from two, three or more different sources – each looking at the same area of assessment BUT from a different window. These sources are direct observations, video observations, case studies, conversations with colleagues (MSF. CSR & ESR), conversations with patients (PSQ) and so on.
How does WPBA work?
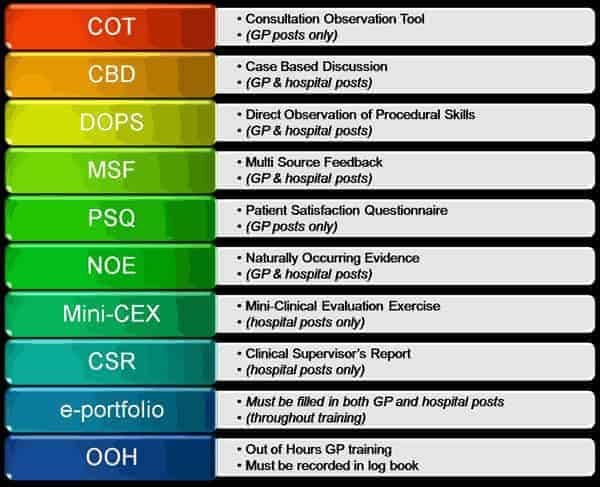
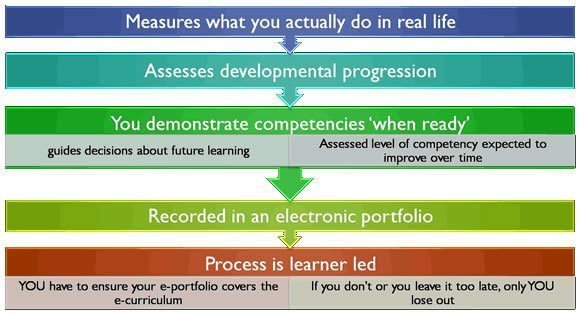
As you can see there are lots of different types of WPBA. And more will be added as the years go by and the RCGP decides what other elements need testing. The process is outlined in the infographic above. In summary… you decide when these assessments take place (usually when you feel you are ready), but don’t overlook the minimum number you have to do in each post. And remember, minimum numbers are MINIMUM – you should be aiming to do lots more!
- WPBA will look at YOUR relationships with colleagues and with patients. It will look at things like continuity of care, patient centredness, empowerment and patient satisfaction .
- The WPBA tools are designed to capture evidence of performance in a structured and formative (developmental) way. It is important to note that there is no pass/fail standards in any of these work-place based assessments. The tools simply serve to harvest information and provides the supervisor with material for feedback and identification of learning needs.
- Therefore, not reaching the required standard in one element of WPBA does not necessarily lead to failure of WPBA. Because there is an overlap in some of the competencies being tested by the different components of WPBA, poor performance in one component will result in looking for the those competencies in the other components to see if you made up for it there; they look at the overall picture.
- So don’t be disheartened if you get an “NFD” grade – instead, see it as a positive opportunity – that you have identified an area that needs working on.
3 important points about WBPA
- RESPONSIBILITY
It is the responsibility of the trainee to ensure that they complete the appropriate assessments and build up a record of their training and evidence of competence AT THE APPROPRIATE TIMES through the ePortfolio. It will be the trainee who tells their trainer/hospital consultant when they are ready to do a specific type of assessment (not the other way around). So, if by the end of your post you do NOT have enough in terms of numbers, the responsibility will be placed solely at your feet and not the trainers.
This is considered fair because once you are working independently as a GP, you will be engaged in lots of other non-consultation stuff like Appraisal, CCG meetings etc and there will be no-one there to remind you. You have to manage all the things on your plate by yourself. You will need to develop your own personal work management system – and it seems right for that to start at the GP training level with WPBA. - NEEDS FURTHER DEVELOPMENT
In your first few posts you may see your trainer or supervisor awarding you a “NEEDS FURTHER DEVELOPMENT (NFD)” grade. Please do not be alarmed by this and do not see ‘needs further development’ as a failure. We expect you to have quite a few ‘needs further development’ especially if you are in ST1 or ST2. If you had all “competent” or “excellent” grades in ST1 or ST2, we’d be worried – how can you have no learning needs at such an early stage in your training. Can you see that if you were awarded a competent grade in everything you do at such an early stage – then there would be no point to training! - HELP YOUR HOSPITAL CONSULTANTS
Some of your hospital colleagues may not be that familiar with what they are doing in the GP training assessments. You can spot who they are – they’re the ones that award you an ‘EXCELLENT’ grade at early on in your training for nearly everything. It’s not their fault – because they have trained to become a consultant, not a GP and in fairness to them, most Deaneries have not trained them up like they way they have with your GP Trainer.
It also doesn’t look good at ARCP time when we see your assessments at the ST1 or 2 stage and everything looks “EXCELLENT” – you can’t be EXCELLEMNT at everything and therefore a whole list of EXCELLENT grades then tells us that those grades are unreliable. So, in order to avoid this (and also whilst we await the training of consultants) we would urge you to attain a good level of understanding of how the assessments work and what each domain or competency means so that you can help your consultant decide what grade to give you by sharing with them what grade you think you should be awared. In this way, we are sure that your hospital colleagues will get the hang of them in no time and it will really help you to get the best out of these. So, please help them to help you.
More guidance
- You should expect that many assessments will be delivered during protected (tutorial) time.
- You need to bear in mind which assessments need to be completed in each post and be responsible for organising them. You decide when these assessments take place.
- Pace yourself; your trainer or hospital consultant will not appreciate it if you try and fit all the assessments into the last few weeks of your post.
- Give your trainer or hospital consultant adequate notice (“Can we do a CBD next week?”).
- Preparation is either necessary or strongly advised: for instance, case selection is very important, as different cases will allow demonstration of different competences, and you need to cover all of them to complete WPBA.
In the early stages of training (ST1/2) it is unlikely that the GP trainee will be able to provide evidence of readiness to practise. The structured evidence, considered against the competence framework, will highlight the areas where the trainee is doing well and those areas where more learning and support is needed. Thus each of the reviews will lead to a learning plan designed to enable the trainee to collect more evidence of competence and to build up a richer picture of readiness for practice.
The standard against which the the trainee is judged is always the level of competence expected of a doctor who is certified to practise independently as a general practitioner. This standard is used throughout the three years of training. This means that in the first two years of training the trainee is being judged against the standard they should have reached at the end of training. Inevitably there will be less evidence from the application of the WPBA tools in the first two years of training, and more developmental needs will be identified. This is what the assessment system is designed to do, so that further training experiences can be directed toward the developmental needs of the trainee. The GP trainee must show competence in all twelve competence areas by the end of year 3.
In 2019, things are going to change. You will be assessed against the expected performance from a GP trainee at the same level as you (ST1, ST2 or ST3) as opposed to a ready to practise qualified GP.
Assessment of competences is about making a qualitative judgement not a quantitative one. We would expect that at the end of ST3 the trainee will have several sets of evidence in each competence area, collected from a range of settings and through different tools. However, the only requirement is that there is enough evidence to enable the trainer to feel confident that the trainee is competent to practise.
Each portfolio will look slightly different, but it should provide a rich picture of competence built up over three years. The “ticks” in the ePortfolio are simply a way of keeping a shared, transparent and systematic record of evidence.


