- Dr Mike Tomson
- Last modified: 31st July 2023
- 2 Comments
Ethics, Diversity & Planetary Health
Planetary Health
DOWNLOADS
path: SAVING OUR PLANET
WEBLINKS
- Podcast by YORLMC – planetary health
- Podcast by YORLMC – greener practice
- www.greenerpractice.co.uk
- https://sustainablehealthcare.org.uk
- MedAct
- SlowMedicine
- – slow medicine calls for more balance, countering the over-emphasis on fast processes which reduce quality.
- WorldMapper – explore the world as you have never seen it before.
- Danny Dorling on Human Geography
……………………………………..
Information provided on this medical website is intended for educational purposes only and may contain errors or inaccuracies. We do not assume responsibility for any actions taken based on the information presented here. Users are strongly advised to consult reliable medical sources and healthcare professionals for accurate and personalised guidance – especially with protocols, guidelines and doses.
COME AND WORK WITH ME… If you’d like to contribute or enhance this resource, simply send an email to rameshmehay@googlemail.co.uk. We welcome collaboration to improve GP training on the UK’s leading website, Bradford VTS. If you’re interested in a more active role with www.bradfordvts.co.uk (and get your name published), please feel free to reach out. We love hearing from people who want to give.
……………………………………..
What you will learn from this page
Aim
- To provide in one place an introductory guide to planetary health focused on the needs of GPSTRs in UK
Objectives
- To introduce key concepts of planetary health which are in RCGP curriculum
- To review ways in which climate change impacts Human health
- To review ways in which GP provision of healthcare impacts on the wider environment
- To suggest areas of healthcare which can be improved where improvement will also reduce the damage healthcare does to the environment
What is Planetary Health?
The RCGP topic guide Professional topic guides uses “the health of human civilization and the state of the natural systems on which it depends” as the definition of Planetary Health. Planetary health looks at health and healthcare through numerous lenses and at the interactions between mankind’s actions, our health, and the impacts of our healthcare processes.
Climate change is probably the best known aspect of how humans have affected our planet and has many effects on human health but the stability of life on earth also depends on ensuring we do not exceed the ecological ceiling on: Chemical pollution, freshwater withdrawal, biodiversity loss, air pollution, nitrogen and phosphorus loading, ozone layer depletion and ocean acidification amongst other factors. (Kate Raworth: Doughnut economics)
https://doughnuteconomics.org/tools-and-stories/11

Why is it important to us? How is it relevant to me as GP trainee?
Planetary health can be thought of as the overarching determinant to human health. Human beings depend on planetary life support systems for our health and wellbeing and ultimately our survival. It is essential that we understand how our natural systems interact with human health determinants.
In addition, the process and delivery of healthcare has a carbon footprint,in the UK this is 4% and the largest public sector emitter.
The waste that we create in healthcare, especially pharmaceutical waste and single use plastics, are hard to break down. Pharmaceuticals are commonly found in our freshwater system where they affect plants and animals.

Primary Care Emissions
The biggest carbon emission hotspot in primary care is medication, with the largest proportion of our carbon footprint coming from what we prescribe. The NHS has been focussing particularly on metered dose inhalers (MDIs) which make up the largest proportion of the primary care carbon footprint (there is a detailed and separate section on these below).

In contrast, estimates from a specialist assessor of primary care carbon footprints (SEE sustainability) suggest that only 0.5% of our carbon footprint relates to waste disposal.
So it’s important to note that the biggest impact we can have as GPs and GP trainees is reducing clinical emissions, avoiding over-medicalisation of patient problems and promoting self-care/patient health literacy. .
Solving clinical issues and the impacts of medication is an issue which often requires action during consultations and also requires a whole team approach. There may be many different interventions needed.
It’s important for primary care to address non-clinical carbon too – things like buildings, waste and staff or patient travel. This may be more appropriate for managers to address.

RCGP curriculum and planetary health
A new RCGP curriculum Topic Guide was shared in Spring 2022 which looks at population and planetary health. It replaces one on population health. It is written as a professional guide rather than a clinical guide i.e. it tries to provide a way of thinking about care all the time that we provide it, rather than being a specialist topic.The new topic guide will be eligible for inclusion in the MRCGP tripos of assessment from October 2022.
The chapter is intended to provide several concepts which are useful throughout GP work and though there are facts related to planetary health the intention is not to expect knowledge of the different greenhouse potential of particular brands of inhaler but to help trainees adapt to different ways of seeing their work.
Some of the concepts being introduced include:
1. Planetary Health and complexity
Planetary health reminds us that in complex systems there are multiple interactions, feedback loops and tipping points. We are familiar with this when we consider how the body ensures appropriate levels of sugar through multiple hormonal feedback loops and intracellular loops too, but planetary health takes us to looking at bigger systems involving how humans have affected the world, and in turn are affected by the world.
The concept of complexity and systems theory with multiple factors interacting is something that GPs may be more used to than hospital specialists as we rarely see people with only one condition (e.g. only Hypertension or Diabetes). We are trained to review personal, social and environmental factors which change the impact of diseases and so are familiar with the challenge of adapting the management of different conditions and issues for a patient so that the desired outcomes are achieved.
(Most of evidence based medicine comes from Randomised Controlled Trials, a process which in general avoids dealing with complexity by ruling out participants who have multiple conditions, and helped demonstrate for example which drugs actually work to reduce covid related mortality. Systems theory, in contrast, helps explain why the covid pandemic spread in the way it did and why some interventions worked for certain populations.)
2. Planetary health : two questions to ask
If planetary health is that complex then how can we work with it in day to day practice? One answer to this is to look at two questions:
- How does planetary health impact on this patient’s or population’s health?
- How does patient or population management impact on planetary health?
So for a person being seen in a GP practice with a diagnosis of asthma we might use the first question to think about the extent to which factors like air pollution from traffic or local industry or mould in their housing are causing the level of asthma they are experiencing. When looking at the second question we’d consider whether the inhalers they are being prescribed have been chosen to reduce the amount of greenhouse gases they emit (Metered dose inhalers contain propellant gases approximately 1000-3000 times as powerful as CO2 whereas dry powder inhalers do not contain propellant gas and have a much smaller carbon footprint).
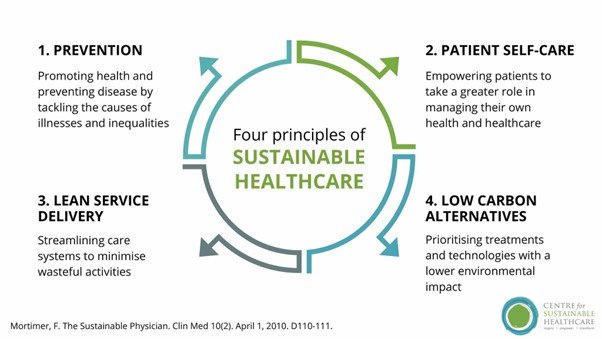
3. What are the principles of sustainable clinical practice?
The topic guide chapter on planetary health suggests that we can consider how to make our practice more sustainable by examining our work through the lens of the four principles of sustainable clinical practice

4. Inequality, health and justice
It is a recurrent finding in planetary health that the impacts of harm created by humans to the planet impacts disproportionately those who have the least resources.

This applies both at an international level (the poorest countries and the poorest people in them generally suffering most from climate change for example) and locally where the poorer people are more likely to suffer economically or from air pollution.
This is in keeping with Tudor Hart’s inverse care law
“The availability of good medical care tends to vary inversely with the need for it in the populations served. This inverse care law operates more completely where medical care is most exposed to market forces and less so where such exposure is reduced.”
There is more information on health inequalities and climate here https://www.greenerpractice.co.uk/information-and-resources/health-inequalities/
So what are the impacts on Human Health of climate change?
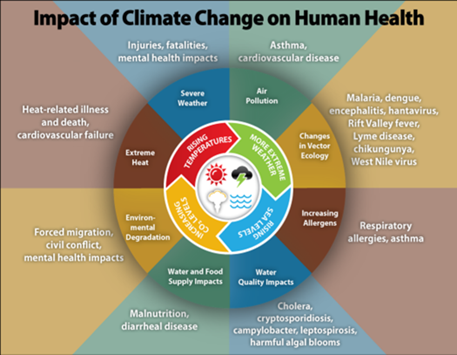
Air Pollution
Air pollution is associated with approximately 7 million premature deaths worldwide, or 40,000 premature deaths per year in the UK according to the RCP. It is also associated with a wide variety of morbidity (which is not limited to respiratory illnesses.)
Air pollution is related to a variety of different pollutants. Particulate Matter is one part of this and is categorised by the size of the particles with bigger ones of 10 nanometres or more (PM10) causing primarily nose and throat irritation and smaller (PM2.5) ones getting absorbed into cells and causing significant changes there.
Other key air pollutants are Nitrous Oxides, Sulphur dioxide Carbon monoxide and Ozone . As many industries and vehicles produce a mixture of air pollutants it is hard to separate out the effects of each component of air pollution, especially as together they are more likely to produce ozone and so additional effects.https://www.cleanairhub.org.uk/clean-air-information/the-basic-information/what-is-air-pollution
Different sources of air pollution will have different balances of pollutants…

Data from 2021 shows that 35% of NOX and 13% of PM2.5 come from transport https://www.gov.uk/government/statistics/transport-and-environment-statistics-autumn-2021/transport-and-environment-statistics-autumn-2021
The move to more electric cars will reduce NOX but as they will still produce tyre and brake emissions there is expected to be much less reduction in PM2.5 related to them.
Air pollution has impacts on every organ in the body. Effects range from direct impacts on respiratory conditions to long term impacts on cardiovascular disease, with more heart attacks and strokes being associated with areas of high air pollution. Importantly air pollution can also impact children’s development, our fertility and our risks of diabetes.There are of course also effects on plant and animal health. Air pollution affects biodiversity.

There is a common assumption that when you are inside a car with your air conditioning switched on then you are safe from air pollution. However, research suggests that in car air pollution is a significant issue and that pollution will build up from neighbouring cars and the car gradually develops higher concentrations of pollutants than outside. https://www.rac.co.uk/drive/news/motoring-news/in-car-pollution-equivalent-to-passively-smoking/ This should be an encouragement to active travel and to use the backroads when walking to minimise exposure.
Domestic log burners are another preventable source of air pollution especially as they cause pollution inside the house they are fitted in and spread pollutants to the downwind neighbourhood. A good source of information on what you can do is through https://www.cleanairhub.org.uk/clean-air-information/what-can-i-do
To find out more about your own contribution to air pollution and ways to address this visit https://calculator.cleanairhub.org.uk/quiz
For more information about air pollution https://www.greenerpractice.co.uk/information-and-resources/information-for-patients/air-pollution/
for actions you can personally take there are great resources from the Global Action Plan Clean Air Hub: What Can I Do about Air Pollution?

Changes in Vector Ecology
Over the last 30 years vector borne diseases like Lyme disease have changed from being localised (in the UK to the New Forest) to becoming endemic. In some ways a more significant example of the spread of vectors is the changing epidemiology of Dengue fever, IN 1970 isolated to only 9 countries it is now endemic in 100. https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue Local transmission has been reported in Europe since 2010.
The risks of vector borne disease spread is changing due to climate change, with the risks growing according to this US based report. https://www.cdc.gov/climateandhealth/effects/vectors.htm
Increasing Allergens
The production of pollen is thought to be increased by longer warmer temperatures and climate change is associated with longer pollen seasons and higher pollen counts. https://www.cdc.gov/climateandhealth/effects/allergen.htm . In addition air pollution is known to increase the severity of allergic rhinitis and allergic asthma exacerbations. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5941124/ explains some of the various reasons though as allergic rhinitis was first described by a Dr who came from Liverpool the association of first diagnosis and pollution should not be a surprise.
Water Quality impacts
There is an accepted increase in all diarrhoeal diseases when temperatures are higher, and these diseases are more common with extreme high or low precipitation. https://www.cdc.gov/climateandhealth/effects/food_waterborne.htm
Water and Food Supply impacts
There is substantial evidence that there has been an enlargement of deserts in North Africa. Elsewhere storm damage is making other areas less reliable for agriculture. The immediate effects on UK agriculture might be small but availability of food especially for people from vulnerable groups and areas of deprivation is related to world prices rather than local production, as demonstrated during the Ukraine war 2022- https://www.bbc.co.uk/news/business-61036715 or https://www.aljazeera.com/economy/2022/4/8/food-prices-soar-to-record-levels-on-ukraine-war-disruptions
Environmental degradation
Some environmental degradation is caused by climate changes e.g. the salination of coastal areas in countries like Bangladesh due to breaches in sea defences removing agricultural land or the increasing heat causing spread of desert in North Africa and increasingly in Southern Europe too.
Carbon dioxide is a major driver of the greenhouse effect which causes climate change; it also has a direct effect on oceans. The higher the concentration of CO2 in the atmosphere the more CO2 will get absorbed in oceans where it acidifies the ocean. Increased ocean acidity affects the ability of marine life to thrive. Increased acidity will affect all sea life which has a shell from corals to shellfish. https://www.nhm.ac.uk/discover/what-is-ocean-acidification.html There is concern (but mixed evidence) that increased acidity may also affect the phytoplankton which produce much of our oxygen and are responsible for much of the marine food web.
Other degradation is related to man’s activities (so part of planetary health) but separate from climate change. This includes plastic and other rubbish. From a health perspective though this also includes many pharmaceuticals which do not get broken down in most sewage systems. https://www.greenerpractice.co.uk/information-and-resources/events-webinars/past-webinars/sharon-pfleger-medicines-and-the-environment-25-05-22/
Direct effects of heat on health and health systems
Heat is seen as a silent killer as the deaths are often only identified retrospectively but the effect of increasing heat is well demonstrated. The effects are most prominent in those who are vulnerable (poor or homeless, elderly or frail, children, those who are pregnant) Other groups like those who work outside or in more manual jobs are also disproportionately affected but anybody can be affected.
The effects of heat are related to both its duration (including overnight changes) and its intensity. https://www.who.int/news-room/fact-sheets/detail/climate-change-heat-and-health
Though some of these effects are directly from the heat others will be either mediated by or exacerbated by medications which people are taking. Heat causes vasodilation as a response which is why it causes increased circulatory strain; many drugs will also cause vasodilation (Hypertensive drugs) or work on fluid balance (diuretics) and the combination with heat can be predicted to increase risk. Possibly one response to more UK heatwaves may need to be greater flexibility on when some people take some of their drugs.

Severe Weather
Severe weather (floods, storms, fires etc.) may cause immediate deaths and injuries from the event. Their effect on infrastructure (including health buildings and wider infrastructure) will also cause issues with water provision (and so related health risks), electricity and heating.
Longer term effects from immediate experience of extreme weather range from the psychological impacts of weather emergencies like PTSD and depression through to the impact of mould or the economic impacts of the loss of or damage done to property and possessions.
It is important to note too that those not immediately affected by climate emergencies may be affected by climate anxiety as a result of increased awareness of the risks from climate changes. The effect of this on younger people is particularly noticeable. https://www.thelancet.com/journals/lanplh/article/PIIS2542-5196(21)00278-3/fulltext
At a planetary level severe weather events are a major cause of migration as the physical changes make agriculture or sustaining life harder in so many parts of the world. Migration is then linked to disputes about access to resources and unrest becomes more common. One of the resources that migration will affect is access to healthcare though access to shelter, food and water may be more immediate concerns.
Inhalers
The first priority when treating respiratory illnesses should be to ensure that the patient gets high quality care which will improve their symptoms and provide control of the underlying disease. So the first priority is to follow approved guidelines.
Inhalers are an important source of greenhouse gas emissions and have been counted separately from the rest of medications by the NHS when analysing our carbon footprint. (Anaesthetic gases are similarly separated out for special attention.)
The UK is an outlier within Europe when we look at the type of inhalers used, as in UK approximately 70% of inhalers prescribed are pressurised metered dose inhalers (pMDIs). In comparison in Sweden 13% of the inhalers used are pMDIs. The UK also has a higher death rate from the care of patients with asthma than neighbouring countries which suggests that our use of pMDIs cannot be justified by any claim that we provide better care. Though GPs have adjusted to ensure that all those treated with an inflammatory condition like Rheumatoid arthritis are treated with a disease modifying drug we have a lot less success in promoting the same approach to asthma where disease modifying preventers are under-used. National guidance is that anybody who uses 3 or more SABA inhalers in one year has poor control and needs review. So focussing on improving care for those overusing their inhalers can be a good place to start improving outcomes whilst also improving the impact on the planet.
Possibly the quickest gain on inhalers is through asking patients to bring all their used inhalers ( and other medication) to the pharmacy when they have finished it or no longer want it. All inhalers disposed of in domestic waste will either go to landfill where their greenhouse gases will be release gradually or burnt at an insufficiently high temperature to break them down. Pharmacists have a legal duty to collect unwanted medication and to ensure it is appropriately destroyed. https://psnc.org.uk/national-pharmacy-services/essential-services/disposal-of-unwanted-medicines/
To reduce the carbon footprint of inhaler prescribing:
- Optimise asthma and COPD care following national guidelines.
- Offer dry powder inhalers or soft mist inhalers as first choice when clinically appropriate.
- If pMDIs are needed for an individual then chose brand and regime with care to minimise
- carbon footprint.
- Ask patients to return all used or unwanted inhalers to community pharmacies or
- dispensaries for disposal by incineration or recycling.
To safely and effectively change inhalers:
- Focus on finding the right medication and device for each individual in consultation with
- them and their carers, through shared decision making.
- Assess and optimise inhaler technique at every opportunity.
- Follow patients up to ensure suitability of device and disease control.
- Do not undertake blanket switching if changing the device type or medication.
This and much more advice on how and why to address inhaler issues is available here: https://s40639.pcdn.co/wp-content/uploads/Reducing-Carbon-Footprint-of-Inhaler-Prescribing-v3.3.2.pdf
For more detailed practical advice on how to approach asthma and inhaler issues the Greener Practice website has a wide range of information but also has a series of stepped quality improvement approaches ( including some developed with GPSTRs specifically in mind https://www.greenerpractice.co.uk/high-quality-and-low-carbon-asthma-care/
Clinical changes to reduce carbon impacts
Evidence from Greener NHS has consistently shown that most of the carbon contribution of primary care is from the medications prescribed. So most of the changes that need to be made are clinical ones.

Over diagnosis and Over Treatment
The RCGP overdiagnosis group define overdiagnosis as “the application of diagnoses and treatments which are of little or no value to patients or cause net harm”. This definition reminds us to start with what matters to the patient and so links to the Principles of Sustainable health care and the importance of ensuring patient engagement. It reminds us that we need to move from the traditional medical model of “what is the matter with them” (which focuses on the possible clinical or pathological medical model approach) to a collaborative approach embodying “what matters to you” https://www.whatmatterstoyou.scot/
There is therefore a role for GPs and GPSTRs to be thinking and discussing with patients whether the diagnoses previously reached are helpful and useful, and whether these diagnoses should be treated. For example an old diagnosis of ‘asthma’ from a visit to a junior team member in A&E several years ago which has not been followed up and reviewed is likely to risk causing overtreatment, or a diagnosis of hypertension made many years ago on the basis of a single reading followed by many normal readings since . The RCGP overdiagnosis group report to council shares examples of where screening for dementia or the thresholds for treatment of diabetes etc have caused overtreatment https://www.rcgp.org.uk/-/media/Files/Policy/A-Z-policy/2015/C72-Standing-Group-on-Over-diagnosis—revise-2.ashx?la=en
For further discussion and information on overdiagnosis the Greener Practice site has this: https://www.greenerpractice.co.uk/information-and-resources/clinical-considerations/over-diagnosis-and-person-centred-medicine/
Multiple medications
The more different medications a person takes the greater the chances of there being an interaction, and the more likely it is that one medication is being taken to manage the side effects of an earlier one. In this situation assessing the Anticholinergic burden of those on multiple medications will help patient and Doctor to reassess how useful the current package of medication is for improving duration and quality of life.
In addition studies of non adherence or non concordance suggest that as many as 50% of patients with chronic illnesses may not take their medications consistently. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6045499/
Yet many of these patients will collect their prescriptions ( and so the climate / carbon damage is done) and many of them will also become ill if they do get admitted to hospital or care facility and start taking all the prescribed medication. So there are great health gains AND carbon gains to looking with patients at how they take their medication. There are more examples of how to approach this at a personal or team level here https://www.greenerpractice.co.uk/information-and-resources/clinical-considerations/prescribing-and-deprescribing/
Alternatives to tablets
Historically for conditions such as anxiety and depressions we have commonly prescribed tablets such as antidepressants. However, there is mounting evidence to suggest that this is not the best treatment for everyone. We are currently overprescribing, especially given talking therapies should be offered as first line or alongside medication if necessary https://www.nice.org.uk/guidance/ng222/chapter/Recommendations#treatment-for-a-new-episode-of-more-severe-depression and have been shown to be effective.
There is growing evidence to suggest green and blue prescribing (involving green spaces and water respectively) will improve mental health and that social prescribing involving time outdoors and in company of other people is particularly effective though this remains an area where more research is needed https://www.mdpi.com/2078-1547/10/1/9
It appears and is likely that the inverse care law applies here and the availability of good green and blue prescribing is in general less available in the areas which need this availability most.
Co-benefits
There are co- benefits in changing our approach to prescribing from one dominated primarily by tablets to treat the conditions doctors have found to an approach of treating what the patient is worried about and doing this when the evidence supports this and it is possible with green or blue prescribing. There are several other ways in which it is possible to improve health for the population and improve the health of the planet. Getting a double benefit
Diet
GPs have known for some time that diet makes a big difference to the risk of non communicable disease like Diabetes, ischaemic heart disease and risk of cancer. https://www.thelancet.com/article/S0140-6736(19)30041-8/fulltext . The key risks have included the Sodium content of food ( largely found in processed food) and the lack of grains, of vegetables and of fruit. So there is a strong argument from a pure medical aspect for a change in diet to reduce our risk of these non communicable diseases. There are also concerns about the impact of meat on our health especially if it is processed (like salami etc.) or red meat. https://www.bowelcanceruk.org.uk/about-bowel-cancer/risk-factors/reducing-your-risk/diet/
The graph below shows 77% of our agricultural land is devoted to livestock production but that the amount of calorific value from this (and the amount of protein) is much lower than this at 17% and 33% respectively. So livestock production is a very inefficient way to produce either food energy or protein. (Some of the land allocated to agricultural use in this calculation will be for growing the soya or other vegetables that they eat much of the time).

The Eat Lancet forum https://eatforum.org/eat-lancet-commission/ is an expert based collaboration to advise on how to both reduce the damage to our health from eating foods which harm us and to improve the consequences for the planet of a more balanced diet.

It does not recommend the absolutist approach of everybody becoming vegan but does encourage us to change our diet… to improve our own health and to reduce the risks to the planet of our current agricultural approaches.
There are other planetary health reasons to raise concerns about current factory farming especially of animals, including the use of antibiotics as growth promoters, the effluent from farms and the difficulty in processing this such that run off is causing damage to surrounding areas, ( e.g. https://www.theguardian.com/commentisfree/2022/jun/10/factory-farming-british-river-sewer-wye-chicken-factories ) and the methane produced by cows in particular through their digestion.
There is, unsurprisingly, a justice issue here too. The diet richest in meat and processed foods is found in those who are richest who are in effect ensuring that those who are less well off have less ground on which to grow the food which they need to survive.
more information on agriculture and how to improve biodiversity from WHO https://www.who.int/publications/i/item/guidance-mainstreaming-biodiversity-for-nutrition-and-health
Active travel
There is enormous evidence for the health benefits of physical exercise. If we were to consider the improvements from regular exercise in the same way that we look at the effectiveness of a drug we would be prescribing exercise all the time. There is strong support for exercise from the NHS https://www.nhs.uk/live-well/exercise/exercise-health-benefits/ The description here is of 150 minutes of physical activity spread through the week.
The evidence suggests that incorporating this into normal daily life works best rather than having another thing to have to do. This leads to suggestions to replace where possible trips in cars with walking or cycling… or to only drive part of the way and walk the rest so that the activity is built into a daily commute for example.
Exposure to air pollution is also lower if you are walking or cycling rather than by car and engagement with natural spaces too becomes more possible ( though obviously not on all routes).e cycles are increasingly common and some local authorities enable a period of borrowing one to help people establish if they can engage with this as a way to incorporate cycling and being outside into their life. There are charities and organisations which will adapt trikes and bikes for use by people with a significant variety of illnesses or disabilities https://www.cyclescheme.co.uk/community/round-ups/round-up-bikes-for-those-with-mobility-issues and the UK government has schemes enabling people to purchase cycles or e bikes through their employer ( NB not available to GP partners) https://www.gov.uk/government/publications/cycle-to-work-scheme-implementation-guidance
By reducing the use of cars patients and doctors are reducing the consumption of hydrocarbon fuels and so reducing greenhouse gas, and improving their own health (possibly needing fewer prescription drugs) and avoiding air pollution… multiple health benefits


Engaging with nature
There has been a wide range of work looking at the impact of nature on health. Work has demonstrated that greener front gardens reduce stress for example https://www.sheffield.ac.uk/landscape/news/scientific-research-shows-greener-front-gardens-reduce-stress though this is only one example of research looking more broadly at the impact of improving wellbeing through urban nature https://www.sheffield.ac.uk/landscape/news/invest-parks-and-green-spaces-boost-wellbeing-across-city-say-researchers
Much contact with nature is going to be linked to or overlap with increased physical activity so the benefits will combine.
Non clinical GP
Approximately 40% of a practice’s carbon footprint will come from non clinical areas ACCORDING TO Health care’s response to climate change: a carbon footprint assessment of the NHS in England so it is important to look at how these can be addressed as well as dealing with the very complex area of how to reduce clinical carbon.
Different practices will have different priorities and possibilities dependent on their buildings, size and structure etc. So it can be very helpful to start by measuring the carbon footprint of the practice and using this as well as the areas that members of the team want to work on, (or need to address for other reasons) to define where to start when reducing carbon. There is a free carbon footprint package designed for primary care. Carbon Footprint
The example here is of an actual practice which was assessed by SEE Sustainability , but as each practice is different it should not be read as definitive.

The Green impact toolkit for health https://www.greenimpact.org.uk/giforhealth offers a wide range of small projects designed to help practices both achieve a lower carbon footprint and to enable them to win awards from bronze to carbon! Each project is designed to link to one or more UN Development goals and they do not have to be taken in any particular order. The majority( though not all) of the projects relate to non clinical carbon.
Travel
The balance of travel will vary from practice to practice and the graphic above (from SEE Sustainability) depending on the size of the practice and the type of practice. In very broad brush terms in more deprived urban areas it is common for the better paid staff to live outside the practice area and so their travel is a bigger proportion whereas their patients are likely to travel less but the pattern will vary depending on income, housing availability and how built up an area is.
The best way to find out about the travel pattern of your practice is to do a survey of the staff and to look at where patients live and calculate the distance travelled by those who attend.
The covid pandemic forced a rapid change in work pattern with a massive and sudden drop in face to face consultations. It also pushed practices to allow more work from home, though this was not possible for all staff. Some of the changes made at this time have been reversed, sometimes for good reasons, (and sometimes for political ones!)
Changing travel habits and assumptions about the importance of seeing patients face to face (or assumptions about the efficiency of doing most consultations virtually!) will often be a slow process as it requires finding out what assumptions people have and being clear why changes are being suggested as well as finding solutions which work well for all parties.
As employers GP practices are able to offer the cycle to work scheme to enable their employees (NB not partners) to purchase a bike or e bike with tax benefits Cycle to work scheme implementation guidance for employers – GOV.UK There are also often schemes and grants available from local authorities or from ICS (in England) or health boards etc. to support active travel to work. Some practices have done considerable work on their sustainability and community links and their example can help inspire others https://www.fromemedicalpractice.co.uk/sustainability
Buildings and energy
Like much of the UK’s housing stock English GP surgeries have been built in areas which have a substantial risk of flooding. (old NHS Sustainable Development unit data from approximately 2018 gave this as 7.6% of English surgeries with higher figures for Scotland, Wales and N Ireland). So it’s important to start by checking if the infrastructure is in an appropriate place , and will remain useful to provide health care before starting to refurbish the buildings.
We know that much of the carbon cost of our buildings comes from the balance of heating and heat loss, as well as our use of electricity. For each practice it is important to look at the data to know what will be the most cost effective ways forward so using a carbon calculator is appropriate before making major actions http://www.gpcarbon.org/#/
It is appropriate to look at the temperatures that parts of the building are heated to (to keep in line with guidance for patients and staff but also to ensure lowest appropriate carbon impacts) and to ensure that the timing of heating is appropriate. More long term actions will include looking at the insulation of buildings to ensure that this is effective as possible, this is normally advised before changing from gas heating to less carbon intensive air source heat pumps etc. Though written about homes rather than surgeries, Retrofitting the UK’s housing stock to reach net zero provides a useful summary of issues that need to be addressed for smaller buildings.
Some GP surgeries will have space for a wind turbine, or will be able to install photovoltaic cells, though it is essential to check the legal situation for each surgery with their mortgage provider etc. ICS estates teams may be able to help with information about local schemes to adapt premises, or retrofit as will most local authorities.
Waste
Waste is an emotive and challenging area. At a practice level changes can be made through ensuring that there is commitment to reducing , reuse and then if neither of these are possible recycle. The GreenerPractice website offers a range of advice on waste management in primary care along with links to resources Reducing waste in health care – Greener Practice .
Population
There is a body of opinion https://populationmatters.org/ supported by people like Sir Divid Attenborough which argues that a key solution to the planetary health crisis is to control the population of the world.
In general it is completely true to acknowledge that the more human beings there are on the world the greater the number of mouths there will be to feed and the larger the resources used. Therefore it is important that we are able to offer good contraception to all those who want it and good access to a full range of women’s health services.
The area that is associated with a divergence of opinion is how or whether to go beyond the availability of womens’ health services and contraception to encouraging people to have smaller families because of the planet. Planned family sizes are in the interests of both planet and patients; discussion of this is appropriate to have in society. It is important to ensure that the interests of patients remain paramount when they visit their primary care physician.
This links with issues of social justice as the impact of people on planetary health is dependent on where in the world they are born and what their likely income is going to be. In general those in the developed world have very much greater impacts on climate change and on planetary health, indeed the top 1% of the world population are estimated to be responsible for 15% of the world’s total emissions and the richest 10% of people for approximately 50% of world global emissions. https://www.oxfam.org.uk/media/press-releases/carbon-emissions-of-richest-1-set-to-be-30-times-the-15c-limit-in-2030/
Whereas the biggest families are generally associated with poorer countries and poorer families.
So there is a justice issue in looking at reducing the population of the poorer countries in order to address the global emissions associated with richer people (who generally have smaller families.)

One conclusion for those working in UK primary care is to ensure that there is easy access to the full range of women’s health and family planning approaches for all those in the practice area offered in ways which are culturally acceptable.


This is a really helpful and comprehensive look at Planetary Health and should be required reading for all trainees AND trainers!
I didn;t realise how much our activites as dcctors could affect the planet before now