Bradford VTS Online Resources:
Teaching & Learning
Trainee In Difficulty
DOWNLOADS
path: TID
SUPPORT SERVICES
- Learner Support in Yorkshire & Humber
- Counselling services available in Yorkshire & Humber
- Career Choices questionnaire: the Sci59 (is GP the right choice?)
- BVTS pages on financial difficulties
- Practitioner Health website – a service for doctors by doctors
- BMA support services: your wellbeing
- Doctors’ Support Network – peer support for mental health concerns
- GP Safehouse: burnout & mental health
- Forced Marriage help service
WEBLINKS
Trainees or Doctors in Difficulty (TIDs or DIDs)
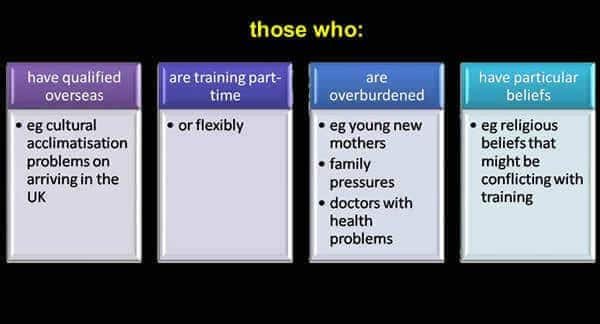
TYPES OF TRAINEE DOCTORS TEND TO EXPERIENCE DIFFICULTY
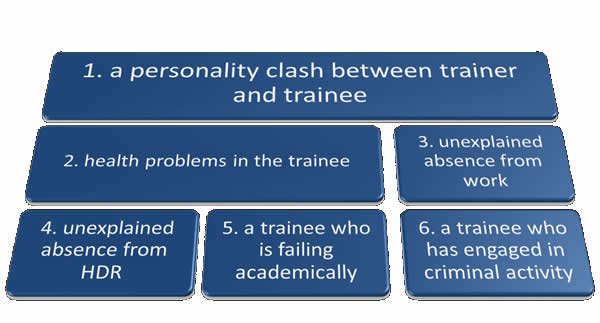
TYPES OF PROBLEMS DOCTORS IN TRAINING EXPERIENCE
If you're a trainee experiencing difficulty...
Please be discuss things EARLY with either your GP Trainer, Consultant, Educational Supervisor or Training Programme Director. If the issue involves one of these people – try someone else on the list. The important thing is to aire your problems early to stop them from escalating to exponential levels. The earlier you talk, the earlier other people can help you. We understand that sometimes trainees don’t feel like wanting to talk for fear of guilt, embarassment, letting people down and so on. We appreciate that talking to us requires a level of openness, honesty and trust but please be reassured that our Clinical Supervisors, Educational Supervisors and TPDs will be sympathetic and understanding. They are caring people.
- Please make contact with you Clinical Supervisor, Trainer, Educational Supervisor and TPD. You will find all of them sympathetic and understanding. Contact them EARLY. Don’t let things brew. If you are then referred to the Deanery’s performance team, please don’t be scared about meeting them. Remember: their job is to try and help you – because they GENUINELY want to help increase your chances of successfully completing the scheme. But before they can do that, you need to be open and honest with them. And they will be open and honest with you.
- If you feel your difficulty is impacting on your health, please make an appointment with your own GP. If you are not registered with one, now is the time to do it.
- If you are unsure as to whether you are fit to work, please make an appointment to see a doctor at your local Occupational Health Department. They are usually based at the local hospital. For Bradford: Employee Health & Wellbeing Manager, Lynfield Mount Hospital, Daisy Hill House, Heights Lane, Bradford, BD9 6DP, Tel:01274228570, Mobile 07432721813. TPDs/Trainers – you can refer via the Occupational Health Referral Template in the Downloads section above.
6 Types of difficulty
These situations should be faced sooner rather than later. Share your concerns with the involved trainee. Try and seek advice from your TPD and perhaps fellow GP Trainers (if at a Trainers’ Workshop – try and maintain confidentiality). A TPD should involve themselves at this stage with the aim of clarifying issues and arbitrating if this is feasible. Every effort should be made to solve this problem quickly at a Scheme level. If the problem seems complicated Deputy Directors are available to advise and guide you and your TPD. It is vital that trainers document their concerns and also share these concerns with the involved trainee – the place to do this is in their ePortfolio (under Educators’ Notes). Do NOT keep hidden external records. The outcome of external arbitration may be to move the trainee to another practice. It is important that neither of the involved people see this as failure. The scheme will have a responsibility to keep in contact with those involved over the following few months to deal with any developments.
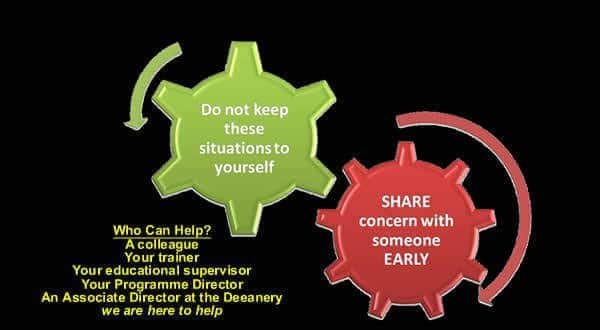
What not to do : Do not keep these situations to yourself. Do not think that the answer is to “sack” the trainee. Do not think the Deanery will sort this out `sometime’.
The important principle again is that you share your concern about your trainee’s health both with the trainee and your Scheme’s TPDs. You should encourage your trainee to have a personal GP who is not based within the training practice. You should document any concerns in the trainee’s ePortfolio (Educators’ Notes). Occupational health services are available for trainees and you should refer them via your scheme for an assessment if you are concerned. It may be necessary for the trainee to take sick leave from work to allow this process to happen. Where trainees lose a period of training due to illness there are now easy mechanisms for ensuring extended training is provided.
In a small number of cases the health problem will be such that it raises doubt about the safety of the doctor to practice. If you have these concerns you should share then urgently with your Scheme and also with your patch’s Deputy Director at the Deanery. The Deanery has clear mechanisms for referral to the General Medical Council. It is vitally important that you have documented your concerns in these situations (again, the place to do this is in the ePortfolio, under Educators’ Notes) as you will eventually have to provide a written report for the General Medical Council.
What not to do : Do not take on the role of becoming the trainee’s personal GP and taking over all responsibility for their health. Refer them back to their own GP.
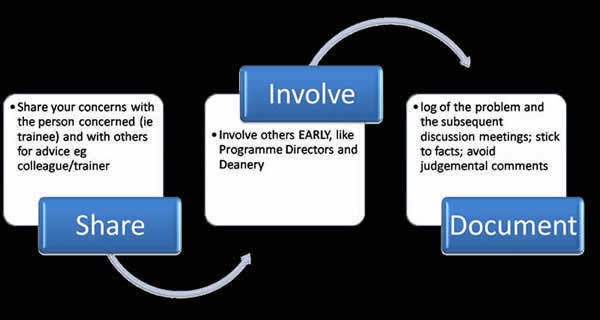
The key words again come into play.
- SHARE
- INVOLVE
- DOCUMENT
You must share your concerns with the trainee at the earliest possible time. Document all concerns that you have (in the trainee’s ePortfolio, under Educators’ Notes). You must involve the TPD at an early stage; they may have to involve the Deanery. If you believe it will be difficult for you to make the decision relating to signing off the Clinical Supervisor’s Report or the Educational Supervisor’s Report then you should share this concern with your TPDs at an early stage too. DO NOT FALL INTO THE TRAP OF SIGNING THE ESR/CSR IN THE HOPE AND BELIEF THAT THE DOCTOR INVOLVED IS CERTAIN TO IMPROVE IN FUTURE POSTS.
Any unexplained absence from work should trigger an attempt to contact the involved GP trainee. “Case Law” usually suggests that there is an underlying problem that has overwhelmed the involved doctor. Be supportive. If you are unable to contact the doctor or unable to undercover a significant problem communicate with your local TPDs who may involve the Deanery. Do not “sack” a GP trainee without discussing this with your TPDs first.
GP Trainees vary in their attendance at half-day release. It may well be that they have identified a more effective personal method for education. They should however have discussed this with you and got your and the TPDs’ agreement. What is not acceptable is absence because they don’t feel like attending. If they are not spending the time, when they are not at half-day release, working in the surgery they are in fact acting fraudulently and action will have to be taken. They are paid to attend HDR. HOWEVER, do remember that absence from HDR may be one of the first signs and symptoms that something deeper and more troubling is happening in the trainee’s life.
As an employer you must follow employment law. All training practices should ensure that the contract that they provide for GP trainees contains sections relating to discipline and is in line with current employment law. Advice about contracts is available from the BMA. In any situation where you have concerns you should share your concerns at the earliest possible moment with your TPDs and with the Deanery. You may have to suspend the GP trainee on full pay whilst investigation is taking place.
Advice for Trainers and TPDs
Dear Trainers, TPDs & Consultants…
- PLEASE talk to someone EARLY to help implement early remediation and stop things from deteriorating drastically. Remember that there are many sources of support for you too.
- One of the people to talk to EARLY is the trainee. The other is as another Educator – like a TPD or the Performance lead at the HEE Deanery.
- A useful mnemonic is SID – Share, Involve and Document. More on this below and the pictorial on the right.
- Start by talking to the trainee – keep them involved right from the beginning. Do not act in haste. Be polite, courteous and show a genuine desire to help and understand. There is no space for hostility. Do you want them to open up and having honest discussions or not?
- Stop and gather more information first. Try and understand the situation – which may involve talking sensitively to others, like admin staff, nurses or other doctors, to help you gather more sensitive ’rounded’ information.
- Consider doing an RDMp assessment to determine what the problem is and help identify causal and maintaining factors (see resources above).
The two people to consider involving are 1) The Training Programme Director and 2) The HEE Deanery’s Performance Lead. Contact the local Training Programme Director. Some GP training schemes have “TPD advisors” – a specific advisor for every GP trainee on their scheme. For example, Bradford has 5 TPDs and about 100 GP trainees. So, every TPD has about 20 GP trainees they are the nominated advisor for – for both pastoral and educational difficulties. If in doubt, contact the Training Programme’s administrator or any one of the TPDs for advice. And depending on how serious things are, the HEE Deanery Performance Team may also need to be involved – again, ask your Training Programme Director.
In terms of advising the trainee…
- Ask the trainee to see their own GP if there are health concerns.
- Suggest the trainee to make contact with a Counselling Service if appropriate.
- If have concerns about the trainee’s ability to perform at work – then think about the Occupational Health Service – which is usually based at the local hospital. Ask your TPD about how to refer. Normally requires a referral form – one which can be found in the downloads section above.
- For contractual or employment issues, don’t forget about the BMA – they have Industrial Relations Officers available to provide free advice. Involve the TPDs and Deanery too (speak to Deputy Director).
- You may need to advise the trainee to call their Defence organisation if they have been involved in a Serious Untoward Incident (SUI). Involve the TPDs and Deanery (Deputy Director).
- Review the list of ‘Support Services’ at the top of this webpage (on the right) – and determine which organisations might be helpful.
If there are serious performance or serious health concerns…
- If there are patient safety concerns, stop the trainee from working (get them to take sick leave) and review the patients they have seen so far to ensure no harm has been incurred.
- BEWARE mindful of not becoming the trainee’s personal GP – refer them back to who their registered GP and retain appropriate distance.
- Inform the TPDs EARLY.
- Ask the TPDs whether they need to involve the Deanery’s Performance Team. They usually need to if there are performance/health/patient safety concerns. They can usually remove the load of making difficult decisions from your shoulders. Do not short-circuit the ladder however, the natural place for Trainers/Hospital Consultants to voice any initial concerns is with the Programme Director(s) and then to ask them whether the Deanery’s Performance Team needs to be involved.
- Consider a referral to the local hospital’s Occupational Health Department: discuss with TPDs first. The best person to do this is the person who knows the trainee the best – and this may be the GP trainer or the Hospital Consultant – but always involve the TPD advisor. Use the Occupational health Template Referral Letter in the Downloads section above.
- Do you need to inform the Responsible Officer for NHS England? Your TPD and Deanery should be able to help make this decision if you ask them. www.england.nhs.uk contact-us or (0300 311 22 33 and ask for the Responsible Officer for GP Trainees).
- Do you need to involve the GMC? Your TPD and Deanery should be able to help make this decision if you ask them.
- Remember – if you are ever worried about a trainee seeing patients, the precautionary principle in relation to patient safety should be applied – i.e. put measures in place to stop them seeing patients until further assessments (e.g. occ. health, own GP etc), clear supervision and safeguards have been applied. And get in touch with the TPDs ASAP – who will advise you further.
Where do I record my concerns about my trainee?
- Rule 1: DO NOT KEEP SEPARATE RECORDS DETAILING CONCERNS YOU HAVE ABOUT A TRAINEE. It’s against the Data Protection Act and you will be fined! A trainee has a right to see everything that is written about them – including emails! If you want to write about the trainee, write it in their ePortfolio and share it with them in advance.
- Rule 2: KEEP THE TRAINEE IN THE LOOP AT ALL TIMES. This means sharing all your concerns with them, and perhaps even documenting them together so that both of you are on the same wavelength or that subsequent dialogue can ensue.
- Rule 3: DO NOT BE HOSTILE. There’s no need for hostility. Aim for and adult-to-adult type conversation with your trainee. If your trainee is being defensive, it’s often because they are scared (wouldn’t you be?). Be open, be honest, be caring and show compassion. Show them that you want to do what’s right for them and get them back on track.
- Rule 4: NOTES FROM MEETINGS AND EVENTS SHOULD GO IN THE ePORTFOLIO. Write things under the ‘Educators’ Notes’ section. This section is open for all who have access to the trainee’s ePortfolio to see (including the trainee). If you’re going to put something potentially emotionally upsetting in the ePortfolio – please consider writing it up in the presence of the trainee (of course, signposting it first). There’s nothing worse than a trainee logging in and finding an unexpected comment which they also find hurtful.
The major key point is to involve all ‘stakeholders’ early. Don’t fret too much over whether you think you are making too much of a fuss or not – it’s better to be safe than sorry! When concerns are passed on late, there is very little space for effective suggestions and alternatives. The hierarchy for involving others would go something like this:
- Talk to the trainee
- Talk to other members of the practice (if appropriate)
- Do an RDMp assessment – to isolate the problem
- Talk to the TPDs
- Inform HEE Deanery – Deputy Director, Doctor in Difficulty (DID) Tutor, Performance Tutor
- If there are health or serious performance concerns refer the trainee to (a) own GP, (b) counselling (c) Occupationhal Health assessment, (d) may need to inform NHS England, (e) may need to inform GMC
- Matters relating to contract and employment – think of the BMA (Industrial Relations Officer)
- Significant Untoward Incident – involve HEE Deanery and Medical Defence organisation.
Making a referral to Occupational Health
- The more detailed the OH referral letter and details the more likely it is to get a useful answer
- Informing the OH department of nature of the trainee’s rotation and expected work helps
- Use the Occupational Health Referral Letter template in the Downloads section above
- At present most referrals are either done by the employer ( e.g. GP practice or employing trust) or by the schemes; the choice seems to be really around who knows the trainee best , and who has greatest need … often the scheme because the concerns are likely to go beyond the current post (and some of the information may need passing on).
- So, in summary, it is best done by the person who knows the trainee the best. This may be the trainer, the hospital consultant or the TPD. However, whoever writes the report needs to collaborate with others who need to input into the report.
- The report is done for the referrer and shared by OH with the referrer and the trainee. Trainees are encouraged to put the OH report on their ePortfolio. However, as it is confidential material it is appropriate not to demand/ expect full release to this open access forum. As it contains personal/confidential information about a trainee’s illness, it is appropriate to allow some editing.
- When making the referral ensure that all other relevant people are informed of the referral and told how to access the report ( e.g. HR dept of future employers, scheme if ref done by GP practice, or GP practice if ref done by scheme, DiD team/ locality office ). HOWEVER, please remember issues around consent to share the report here – which the GP trainee needs to give first. DiD = Doctors in Difficulty.
- The DiD (Doctor in Difficulty) tutor at the Deanery has a role in checking that OH has been used when appropriate and that relevant OH reports are not lost but are seen, followed up and acted on.
- Schemes do have a co-ordinating role in knowing that OH has been referred to and sharing the information which they have ( provided there is consent to share the details… if no consent then sharing awareness that a report has been done).

