Paediatrics
Bradford VTS Clinical Resources
- by Drs Jenny Wright & Cristina Costache
- Last modified: 4th January 2024
- No Comments
DOWNLOADS
path: INFANTS & CHILDREN excluding teenagers (which has a separate folder)
WEBLINKS
- Children & Young People super-condensed curriculum – what you should know (RCGP)
- http://gppaedstips.blogspot.com/ – a great paeds blog
- Dont Forget The Bubble DFTB – modules
- Don’t Forget The Bubble DTFB – blog
- OSCEs in Paediatrics (BVTS)
- https://what0-18.nhs.uk– amazing website for parents and doctors – click professional area for great safety netting leaflets, wonderful clinical protocols at a glance.
- Retinoblastoma – information for GPs
FOR PARENTS
……………………………………..
Information provided on this medical website is intended for educational purposes only and may contain errors or inaccuracies. We do not assume responsibility for any actions taken based on the information presented here. Users are strongly advised to consult reliable medical sources and healthcare professionals for accurate and personalised guidance – especially with protocols, guidelines and doses.
COME AND WORK WITH ME… If you’d like to contribute or enhance this resource, simply send an email to rameshmehay@googlemail.co.uk. We welcome collaboration to improve GP training on the UK’s leading website, Bradford VTS. If you’re interested in a more active role with bradfordvts.co.uk (and get your name published), please feel free to reach out. We love hearing from people who want to give.
……………………………………..
Paediatric basics
- Children make up about one-fifth of the UK population. Caring for them is an important part of a GP workload.
- In the UK, clinical workload in primary care has increased by 9% between 2007 and 2014 among children below 5 years of age.
- Garralda et al defined frequent attendance as four or more attendances during a 12 month period. Vila et al used the same definition, and reported that 30% were frequent attenders. They categorised each child into a usage category: low usage (0–4 visits/year), medium usage (5–6 visits/year), and high usage (≥7 visits/year) for the first year.
- In more recent times children under age 5 are more frequent attending GP surgeries and of these many are frequent attenders.
- Around one-quarter of all patients aged <18 years visit their GP each year, and on average the majority of GPs see around 400–600 children in a typical 6-month period.
- LISTEN TO PARENTS: The carers or parents know their child best and their instinct is usually correct. LISTEN to their concerns.
- PMH & BH: Review the child’s past medical history and birth history as this gives clues to risk factors eg if premature or history of atopy may be more likely to have chronic respiratory problems. It may also inform parental developmental concerns eg. if slow to speak could this be due to ear infections?
- FEEDING & FLUIDS: Ask about feeding / fluid intake and wet nappies (babies and infants can become dehydrated quickly). Red flag if not passed urine or wet nappy < 12hrs.
- PSYCHO-SOCIAL ENVIRONMENT: In chronic problems eg behavioural or chronic illness consider the psychological, social and environmental context – this will impact upon a child’s future health and development. Are there safeguarding issues / parental mental health issues, neglect, poverty and poor housing?
- RESISTANT TO EXAMINATION? Are they alert and active, and resistant to examination? If not this can be a red flag.
- VITALS: Record vital observations on ALL children and have a chart accessible to refer to age related parameters (see NICE traffic light guideline below).
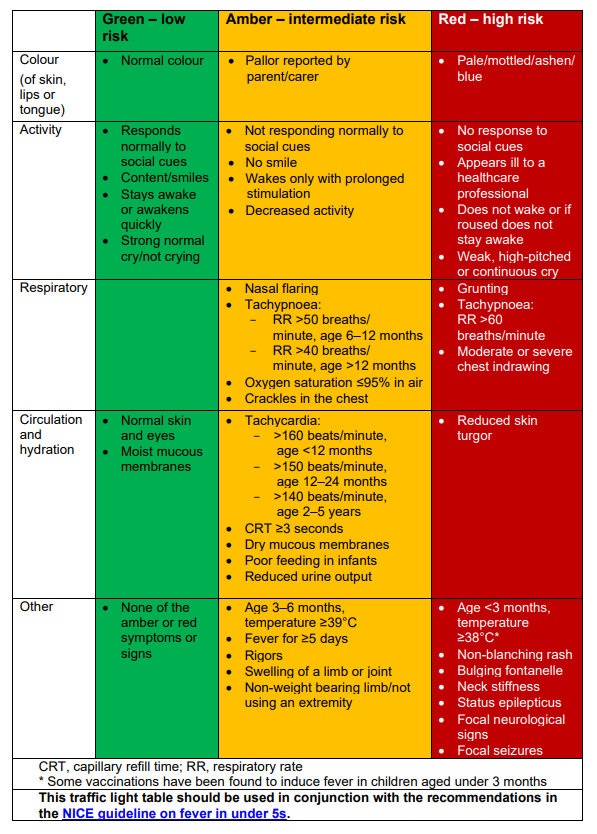
- NICE’s TRAFFIC LIGHT SYSTEM: for identifying risk of serious illness in under 5s – see table right.
- Children with fever and ANY of the symptoms or signs in the red column should be recognised as being at high risk.
- Similarly, children with fever and any of the symptoms or signs in the amber column and none in the red column should be recognised as being at intermediate risk.
- Children with symptoms and signs in the green column and none in the amber or red columns are at low risk.
- The management of children with fever should be directed by the level of risk.
Dr Edward Snelson, Consultant Paediatrician writes… I am often asked if I use the traffic light system in my own practice. The answer is yes and no. Yes – the system is a useful hierarchy of signs and symptoms. No – because most childhood illnesses are too dynamic for a snapshot to be completely valid. Things change constantly. A risk assessment based on a moment in time is far too simplistic. That doesn’t mean that observation of the child is necessary for decision-making. In most cases, it’s simply a question of asking how the lights are changing and what I’m going to do with that.
As babies get older, they’ll settle into a more predictable feeding routine and go longer stretches at night without needing a bottle.
| Age | how much they feed | how often they feed |
| First few days of life | 1.5-3 oz (45-90ml) | every 2-3h |
| At about 2 months | 4-5 oz (120-150ml) | every 3-4h |
| At about 4 months | 4-6 oz (120-180ml) | at each feeding |
| at about 6 months | 6-8 oz (180-230ml) | 4-5 times a day |
Admission
- Of course, you should always admit for urgent medical conditions you are worried about.
- If the child’s safety is in question and there is a safeguarding issue, again admit for their protection.
- However, you should also consider if the parents are heavily worried about their child, even if your worry might not mirror theirs. Paeds are usually happy to accept referrals like these if you explain the intense parently worry/anxiety. Why? Because the parents live with the child 24/7, are the experts of how their child behaves, and their perception might be more accurate than yours. You may well be missing something. And remember, children go up and down – you might seem them at a temporary “well” point.
Much of this section has been taken from Dr Edward Snelson’s paediatric blog because it is, in a nutshell, simply excellent. You can read more about his wonderful blogs here: http://gppaedstips.blogspot.com/
Those of you who have been my GP trainees, will often hear me talk about red, amber and green patients. Red patients are those that are worrying – like those that have features of meningitis. Green patients are those that are not too worrying – like those who simply have a viral URTI. And amber patients are those inbetween – i.e. those that you not quite sure of. An amber patient is not quite worrying as a red patient but also not as reassuring as a green patient.
Those that are red patients are easy to manage – you usually admit them. For example, a meningitis case, you would give benzylpenicillin (or equivalent if allergic) and admit them straight to hospital. Can you see – whilst the condition is worrying, the decision-making involved is easy – you know what to do. Those that are green patients are also easy to manage and again the decision-making is easy. A simple viral URTI = watchful waiting with appropriate safety-netting. But it is in the amber patients where decision-making becomes more difficult. They are not as clear-cut as red and green patients. These are require more complex decision making. Let’s explore this clinical decision-making in a bit more detail.
- First of all think which light the patient is currently at – red, amber or green?
- Then determine, according to their history so far, whether they have changed lights.
RELATIVELY STRAIGHT-FORWARD CLINICAL-DECISION MAKING
- Patient initially started as green and remains green
The decision-making, although it varies on the clinical presentation, is relatively easy. For example, symptoms of a viral URTI which have become a bit worse but you still think viral URTI = watchful waiting + appropriate safety netting. Or someone with back pain as a result of going on an activity trip – with no alarm features – you may suggest analgesia and exercises. - Patient started green and is now red
This is a lot more worrying. You will most probably want to admit. Using the example above – the patient who initially had what sounds like a viral URTI but now is very ill and on examination you think they may have a LRTI. They look so unwell that you feel they need an admission, for IV antibiotics. - Patient was amber but now red
This is the patient who you were a bit worried about but upon review is actually worse. So, take the possible LRTI who you gave antibiotics to, but then comes back a few days later and looks dreadful. Clearly, they need admitting. - Patient presents as red
These always need admitting. The patient who has had three fits today but no history of epilepsy or anything else. Or the patient with meningitis features – you give benzylpen (or equivalent) and admit. The patient who comes in a floppy drowsy worrying state. You get the idea?
- Patient initially started as green and remains green
MORE COMPLEX CLINICAL-DECISION MAKING
- Patient started green and is now amber
This is a bit more worrying. You either want to start treatment and review. For example, the patient who initially had what sounds like a viral URTI but now is more ill and on examination you think they may have a LRTI. If they don’t look to bad for admission, you might start antibiotics and review them in a few days (with appropriate safety-netting should things suddenly turn).Dr Edward Snelson (Paediatrician) writes: A 2 year old child presents with a cough, runny nose and a fever. When you see them they are miserable but alert and interactive. They have a temperature of 39.5, heart rate of 160 and are refusing to drink. They last had any symptomatic treatment 6 hours ago. The parent reports (you have to ask about this – it won’t usually be volunteered) that 2 hrs ago they looked much better and were drinking a bit. Unlike actual traffic lights, unwell children swing from green to amber and back to green quite normally during uncomplicated self-limiting infections. There is a reason that we mostly see unwell children between the age of 6 months and six years. It’s not because they are high risk for dangerous infections. In fact quite the opposite – it is a stage of life characterised by extreme response to simple infections. The normal physiological response can look bad but usually resolves to reveal a reassuring baseline. In many ways, a febrile unwell 2 week old is easier from a decision making point of view – that is a very high risk presentation. A febrile unwell 2 year old is low risk but that presents a different problem – how to recognise the small number that do have a serious illness. What can be terribly inconvenient is the above situation. The snapshot we are given is not green but also not red. Red is also easier from a decision making point of view. Amber presentations make us have to decide what to do next. Here are your options:
- Unwell children will often present with an amber feature which is felt to be related to a lack of symptomatic treatment rather than a sign of serious illness. If that is the case you have the following options…
- Send the child home with symptomatic treatment advice and safety netting advice
- Send the child home with symptomatic treatment advice and arrange remote or face-to-face review later
- Refer the child to paediatrics
- Unwell children will often present with an amber feature which is felt to be related to a lack of symptomatic treatment rather than a sign of serious illness. If that is the case you have the following options…
- Patient was amber and remains amber
This is a very difficult one. You will want to either keep a close eye on the patient (through doing a few more tests, different treatment and a review in a few days time) or admit them. For example, the LRTI that doesn’t seem to be settling despite 3 lots of antibiotics. You might consider an urgent CT or even 2ww if there are other worrying features. - Patient was amber but now green
Generally, you can relax a bit more – the patient seems to have gone through a bad patch and is now settling. For example, those patients who sound like they were quite unwell (and should have seen), but have put off coming to the doctor and actually come in only when their symptoms seem prolonged although a lot better now. So, take the patient who did not present to the doctor earlier, but sounded quite poorly with their chestiness (wasn’t eating or drinking much, found it slightly difficult to breathe, had rigors and chills) but presents to you in the second week because the cough hasn’t gone although they are feeling lots better and their breathing back to normal. So, while you can relax a bit because they seem to be improving, always safety-net because the patient can turn again from their current green status to amber or red at short notice! And this applies especially to infants and children – their colour situation can change suddenly even if they present to you as green.Dr Edward Snelson (Paediatrician) writes: Consider this scenario: A 2-year-old child presents with a cough, runny nose, and a fever. The parent reports that a couple of hours ago they looked pale and lethargic. They were shivering, and felt hot centrally but had cold hands and feet. Now they have none of those things happening. They are walking, talking and cheerfully interactive. This is a very common scenario. Parents and carers will often express a certain paradoxical frustration with the apparent wellness of the child. The child appeared seriously unwell a couple of hours ago and the parent is now feeling that you will think that they have overreacted.
What you can do:- It is a good thing to acknowledge how unwell the child was and use that as an opportunity to..
- Explain why you as a clinician are happy with the child despite how concerning the child’s appearance was.
- Safety-net in case the child turns again. (Consider giving or signposting to something written)
- What you can say: “What you told me about how unwell (child’s name) was earlier sounds quite frightening. It is still very reassuring that they look better now. At this age children respond to infections quite strongly and that can cause some things that can look really concerning. The temperatures can go very high and that immune response causes all of the things that you saw. It’s actually really good timing that they were at their best when I saw them because it allowed me to be able to be confident that it wasn’t signs of something like sepsis or meningitis. Children with sepsis and meningitis don’t do the things your child is doing now. I’m happy for you to continue managing your child’s illness with medicine that make them feel better such as paracetamol and ibuprofen.”
- Patient started green and is now amber
From this, you should be able to see that in terms of CLINICAL DECISION-MAKING,
Green patients are easy
Red patients are relatively easy
Amber patients is where the decision-making complexity lies and requires more careful thought.
- The decision about which strategy to use is influenced by many factors including
- Confidence in the parent/carer ability to seek appropriate reassessment & safeguarding
- Whether you feel it is necessary to have the opportunity to document an improvement in physiological parameters (usually heart rate)
- whether you feel that the child needs another clinician to assess
- Reviews: Every clinician will have a preferred option. Many working in Primary Care do not feel the need to have a face to face reassessment if the child improves in behaviour and activity. That is completely valid as such improvement is a good demonstration of physiological change and evidence that the baseline state of the child (active, interactive, good oral intake and no increased work of breathing) is not consistent with sepsis or meningitis for example.
- Really good safety-netting advice empowers the parent to make that assessment in a way that is dynamic and continuous. A reassessment in whatever form (face to face or remote) facilitates documentation of improvement and adds value to the safety-netting advice by giving the opportunity for the parent to further discuss the illness, what to expect and when to worry. We can equip the person caring for that child with the ability to recognise signs of serious illness should those develop later.
- RULE OF FEBRILE THIRDS – Rule of thirds in paeds for predicting future febrile convulsions in future illnesses in an child/baby who has had one:
1/3rd will not have anymore with future febrile illnesses1/3rd will experience one more
1/3rd will have repeated bouts with future febrile illnesses - Amber children are a fair bit of work but they are a great opportunity to do what we should consider core business. We can take a group of children who are reasonably low risk and look for signs (e.g. increased work of breathing, meningism or unexplained tachycardia) that this one is the one with something that needs immediate intervention. For those that are within what is expected of an uncomplicated infection we can make sure that they have symptomatic treatment in the assumption that they will demonstrate a baseline state of reasonable wellness that effectively rules out serious illness.
- REMEMBER, INFANTS & CHILDREN CHANGE QUICKLY! Paeds is a dangerous specialty because infants and children can be fine one moment and deteriorate rapidly the next (and vice versa!). Therefore, always safety-net: i.e. provide the care-giver (e.g. the parent) information/knowledge of the types of things to look out for and what to do if they occur. Make sure these instructions are clear and explicit. Write them down if needs be, especially if the information is heavy.
- Common outcomes are common but beware of AVAILABILITY BIAS. But do not let common things being common cloud your judgement in terms of not looking for other things. Yes, most kids with a cough will have a viral infection and recover nicely. BUT you are there to assess how they have been and how they are rather than rely on this outcome liklihood alone.
- SAFETY-NET CAREFULLY: Consider parental expectations and concerns and aim to give safety net advice to reassure them and guide them as to when they need to seek further review.
- SEEK ANOTHER OPINION IF UNSURE: If you are unsure what is going on and whether a child needs admission for observation always speak to Paediatrics for advice.
- Trust your instinct!
FUNCTIONALLY DEPENDENT
- Due to loss of function, having impairments of ADLs
- Increased likelihood of requiring addition medical &/or social care
- HBA1c target: 53 – 64mmol/mol
FRAIL
– Combination of significant fatigue, recent weight loss, severe restriction in mobility & strength, increased propensity for falls & increased risk of institutionalisation
– A recognised condition & accounts for 25% of older people with diabetes
– Clinical Frailty scale or CHSA 9-point scale (assessment tool)
– HBA1c target: 60-70mmol/mol
DEMENTIA
– Degree of cognitive impairment leading to sig. Memory problems, a degree of disorientation, or a change in personality & unable to self care
– MiniCog tool (easy to use assessment tool)
– HbA1c target: 60-70mmol/mol
END OF LIFE CARE
- Significant illness or malignancy & have life expectancy reduced to <1 year
- Glycaemic aim – hypo and symptomatic hyperglycaemia avoidance
Medication | Mode of action | Side effects | Cautions (check BNF for more detail) | Dose |
METFORMIN 1st line treatment, unless BMI <25 (23 in South Asian population) Low Hypo risk Reduces CVD risk, weight neutral | Helps to stop the liver producing new glucose. It helps to overcome insulin resistance by making insulin carry glucose into muscle cells more effectively.
| Main side effect if GI affects, generally dose dependent-can be reduced with gradual increase in dose over several weeks or trying modified release Metformin Also: metallic taste, reduced absorption of vitamin B12, build up of lactic acid in the blood, allergic reaction and liver problems. | STOP/DO NOT USE IF eGFR <30 ml/min *Lactic acidosis- care if eGFR < 45ml/min. Document that advice has been given to stop these tablets if they become dehydrated (restart when eating normally again) *GI side effects. Titrate dose slowly to reduce side effects NOTE IF ALT> 3 TIMES NORMAL | Start at 500mg ideally with evening meal, increasing to 1g with evening meal after a week if they have no side effects. Max dose 2 gram over 4 weeks. Consider slow release for to reduce tablet load or if they are struggling with GI side effects.
|
SGLT-inhibitor Empagliflozin Low hypo risk Can help with weight loss | Sodium-glucose co-transporter 2 (SGLT2) inhibitor that prevents glucose reuptake in the kidney, leading to the excretion of excess glucose in the urine. | Polyuria, polydipsia, thrush. UTI, fluid depletion Increased risk of amputation- avoid if h/o leg ulcers | Only start if Cr Clearance > 60. Care if > 75 years. Risk of postural hypotension. Care needed if they have skin ulcers – risk of amputation. Document advice about normoglycaemic ketoacidosis and give ketostix. | Empagliflozin 10mg. Can be increased to 25mg. Expensive so only continue if there is a clear response after 6 months |
SULPHONYLUREA (SU) Glimepiride Risk of hypos Good if rapid response is needed. | They work by stimulating cells in the pancreas to make more insulin. They also help insulin to work more effectively in the body.
| Weight gain. Hypoglycaemia, gastrointestinal side effects, low sodium, facial flushing and intolerance of alcohol, allergies etc.
| Can cause hypoglycaemia, particularly if there is renal impairment or they are elderly. Consider occupation – hypos if not eating regularly, fasting. Make sure you give and document advice about hypos. Make sure they are able to test their blood glucose – issue glucometer, test strips, lancets and sharps bin. (SGBM) Document advice about driving/insurance. | Start at 1mg and titrate up to 4mg depending on glucose level. Should have an effect on Hba1c over a 2 month period. |
GLIPTIN Do not cause weight gain and encourages patient satiety. Although they probably reduce Hba1c levels less than other drug treatments. Low hypo risk | They work by blocking the action of the enzyme, DPP-4, which destroys the hormone Incretin.
| Gastro-intestinal effects, oedema, headache, Avoid if h/o Pancreatitis or heart failure or liver problems. | *Expensive- only continue if they meet NICE guidance. *Not v powerful max likely reduction ~ 11 mmol/mol *Do not use if a h/o pancreatitis *Monitor egfr at reviews *Don’t use if heart failure risk | Linagliptin 5mg if eGFR < 50 |
GLITAZONE Pioglitazone Low hypo risk Consider in people with very significant features of metabolic syndrome. South Asian | Reducing insulin resistance. Improving insulin sensitivity.
| Oedema esp if heart failure or at risk. Rare reports of liver dysfunction. Weight gain, gastro-intestinal side effects, headache, dizziness.
| Discuss with member of Level 2 team before starting. Avoid if they have heart failure or risk of fluid overload Avoid if h/o bladder cancer, undiagnosed haematuria Avoid if fracture risk Monitor LFTs at each diabetic review. Annual urine dip looking for haematuria | Pioglitazone:15mg-30mg. A six month period may be needed to really see an effect from these tablets. NICE recommends that they are only continued if at least a 11 mmol/l reduction in Hba1c is seen within 6 months of starting the treatment.
|
GLP-1 mimetic/insulin | Discuss with Level 2 doctor |
|
- At first warning of episode of hypoglycaemia:
- Immediately treat with a 15-20g of a short-acting carbohydrate such as:
- 200 mls of Lucozade (please note Lucozade formula has changed so lower in sugar- need 200ml)
- 200mls of non-diet drink
- 4-5 glucose tablets
- 3-4 jelly babies
- 200mls of fruit juice
- Immediately treat with a 15-20g of a short-acting carbohydrate such as:
- If the hypo is more severe, and the patient cannot treat themselves:
- applying Glucagel (or treacle, jam or honey) on the inside of cheeks and gently massaging the outside of cheeks.
- if unconscious, Glucagon can be injected if the person treating has been trained to use it.
- Otherwise call an ambulance immediately
- Important:
- If unable to swallow or unconscious, do not give anything by mouth (including Glucagel, treacle, jam or honey). Make sure family and friends are aware of this. If unconscious, place patient in the recovery position (on side with head tilted back) so that tongue does not block throat.
- Follow-on treatment:
- To prevent blood glucose levels dropping again, follow sugary foods with 10-20g of a longer-acting carbohydrate such as:
- half a sandwich
- fruit
- a small bowl of cereal
- biscuits and milk
- the next meal if due
- Patients experiencing regular episodes of hypoglycaemia require prompt review by the diabetes team.
- Severe episodes of hypoglycaemia require urgent review by the diabetes team.
- To prevent blood glucose levels dropping again, follow sugary foods with 10-20g of a longer-acting carbohydrate such as:
Advise patients the following: if you do go down with a cold, flu or any other illness…
- The Basics
- Rest.
- Drink plenty of sugar-free fluids.
- Avoid too much caffeine as this could make you dehydrated.
- Take painkillers in the recommended doses as necessary.
- Contact your GP to see if treatment with antibiotics is necessary.
- If you are vomiting uncontrollably, contact your GP or diabetes clinic.
- Insulin or diabetes medications
- Keep taking your insulin or diabetes medications even if you are not eating. Stop metformin and blood pressure medication if you are dehydrated. CONSIDER AKI SICK DAY RULES – see hypertension protocol.
- Testing
- Test your blood or urine four or more times a day and night (ie at least eight times in a 24-hour period) and write the results down. If you are not well enough to do this, ask someone to do it for you.
- Ketoacidosis
- When diabetes is out of control as a result of severe sickness, it can lead to a condition called diabetic ketoacidosis or diabetic coma if you have Type 1 diabetes. The body produces high levels of ketone bodies causing too much acidity in the blood.
- Testing for ketones
- If you have Type 1 diabetes and your blood glucose level is 15 mmol/l or more or you have two per cent or more glucose in your urine, you will also need to test your urine or blood for ketones. They are a sign that your diabetes is seriously out of control. Ketones are especially likely when you are vomiting and can very quickly make you feel even worse. If a ketone test is positive, contact your GP or diabetes care team immediately.
- Food and drink
- It is important to keep taking your medication as normal and drink plenty of sugar-free drinks. Aim to drink at least three litres (five pints) a day. Try to keep to your normal meal pattern, but if you are unable to, for any reason, you can replace some or all of your meals with snacks and/or drinks that contain carbohydrate such as yoghurt, milk and other milky drinks, fruit juice or sugary drinks such as Lucozade, ordinary cola or lemonade. You may find it useful to let fizzy drinks go flat to help keep them down
Advise patients of the following:
- Vaccinations and/or malaria tablets
- Carry diabetes ID or a GP letter if carrying insulin and list of prescription drugs
- Carry all medication and blood glucose testing equipment in hand luggage
- Consider how to keep insulin cool if travelling for long periods
- Travel insurance: – Allow 2 weeks to buy travel insurance. – Don‟t just buy on price, check the cover and read the small print – – Be honest and declare all medical conditions
- Plan to take twice the quantity of medical supplies normally used
- Consider adjusting medication if travelling across time zones
- Consider adjustment to insulin if travelling to hot or cold climate
- Carry a European Health Insurance Card (EHIC) if travelling within Europe
www.ehic.org.uk, / 0845 605 0707
Consider availability of insulin if travelling abroad for long periods.
Interpreting blood results on pathology template – Remember frailty
- HbA1c <48 →select satisfactory→take no action – patient will be reviewed as per recall
- HbA1c 48-53 →select abnormal →speak to nurse → send task to admin to book tel appt with nurse to discuss abnormal result and document a suggested plan to up-titrate medication based on the above guidance for nurse to discuss with patient – nurse will discuss with patient possible changes to medication and then task Dr back to make changes and issue script. – if on single drug or diet only
- HbA1c <53 → select satisfactory →take no action – if on SU or combination drugs patient will attend at next review 6 months later
- HbA1c >53 → select abnormal (take into account patients age and fraility) →speak to nurse → send task to admin to book tel appt with nurse to discuss abnormal result and document a suggested plan to up-titrate medication based on the above guidance for nurse to discuss with patient – nurse will discuss with patient possible changes to medication and then task Dr back to make changes and issue script.
Any concerns – send message to Level 2 team
Using the SystmOne Template (CDM) for Diabetes.
See CDM review table
- Bloods: U&Es, eGFR, HbA1c, ALT (if first year on statin) and lipid profile – (Consider other tests if have other chronic diseases.)
- Urine ACR.
- BP
- Lifestyle discussion: smoking status/cessation advice, exercise status, alcohol intake, diet.
- BMI
- Retinal review.
- Foot check annually (in house) and record on the template. If moderate or high risk they need a referral to podiatry
- Any complications? erectile dysfunction, neuropathic pain, autonomic neuropathy.
- Hypo unawareness, ? hypos requiring external intervention (see DVLA guidelines).
- Review of blood monitoring – if they require monitoring.
- Medication review: concordance/indications/side effects/if on insulin – injection sites.
- Record medication review done, move date on till next review
- Assign diagnosis to repeat template medication.
- Add/move recall on. NB: Diabetics well be reviewed at least 6 monthly.
TARGETS AT A GLANCE
- BP: <130/80 – particularly if there are renal problems
- Get to non smoking: don’t forget smoking cessation
- Cholesterol: < 4.0mmol/l
- HbA1c:
- Diet alone or single drug not affected by hypoglycaemia <48mmol/l
- Medication <53mmol/l. Patient tailored care needed especially if they are elderly or there are concerns about hypogylcaemia.
- BMI: <25
Diabetes in pregnancy is associated with risks to the woman and the developing fetus.
Planning a pregnancy
Women planning a pregnancy should be referred to a diabetes pre-conception clinic.
Pre-pregnancy planning includes:
- Diet and exercise, weight loss advised if body mass index > 27kg/m2
- Retinal photography unless carried out in last 12months
- Renal assessment (including microalbuminuria)
- Folic acid 5mgs for 3 months preconception and continued for first trimester.
- Establish rubella status, booster organised if required.
- Blood pressure should be monitored
- Smoking/alcohol cessation advice
Review of medications
- Metformin may be used before and during pregnancy, as well as or instead of insulin. The diabetes antenatal clinic will oversee their care whilst pregnant.
- Isophane insulin is the first-choice long-acting insulin during pregnancy.
- Discontinue oral hypoglycaemic agents (apart from metformin), ACE-inhibitors, Angiotensin Receptor Blockers and statins
Gestational diabetes
- 6 weeks post-partum patients require a HbA1c to establish whether glucose tolerance has returned to normal.
- All patients require advice on their elevated long term risk of diabetes.
- All patients require advice on their risk of gestational diabetes in future pregnancies.
- All patients require advice regarding diet, weight control and exercise
All patients require an ANNUAL HbA1c in view of their elevated risk of Type 2 diabetes. Please add an ‘AT RISK OF DIABETES’ recall to their notes.
Specifically Clinical Things
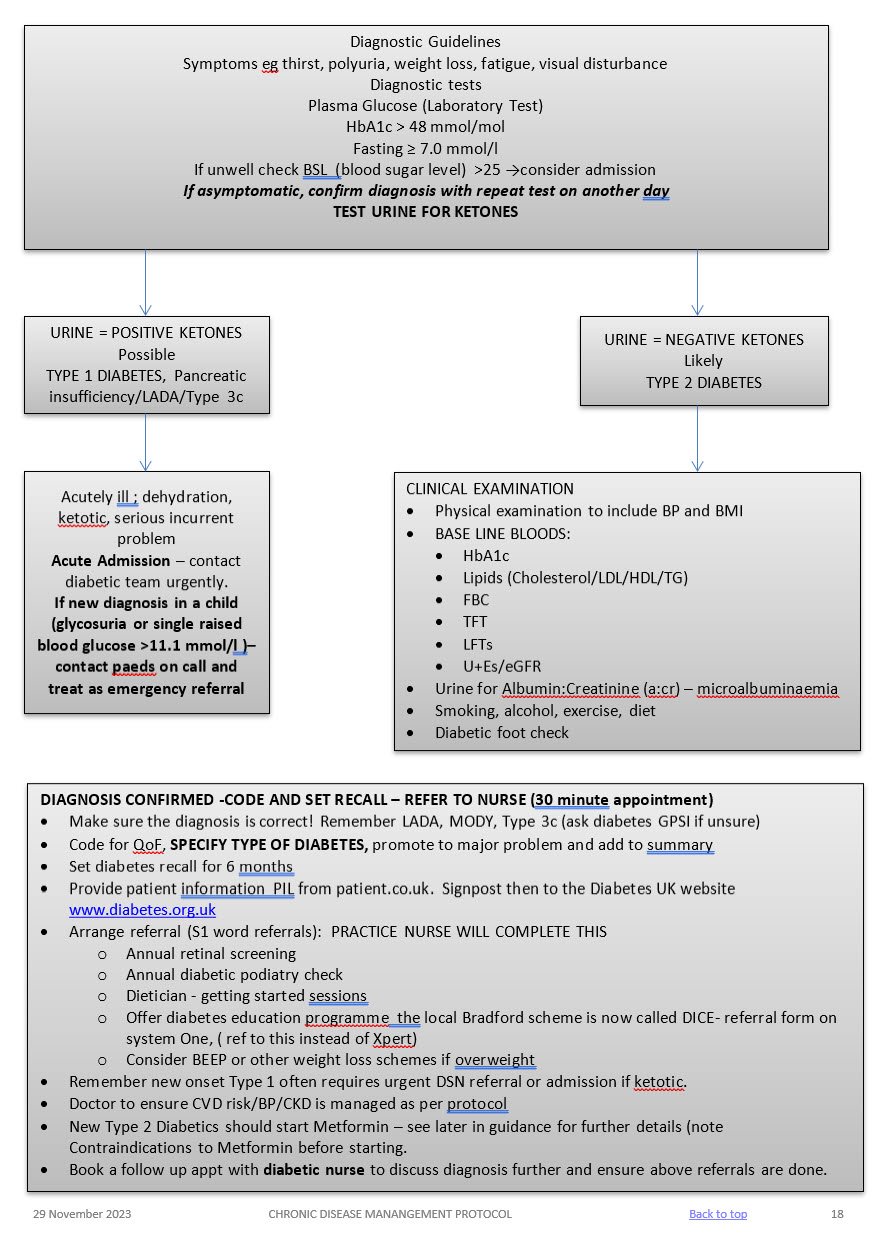
SYMPTOMATIC
Symptoms of hyperglycaemia (polyuria /polydipsia, unexplained weight loss. visual blurring, genital thrush, lethargy) plus either:
HbA1c: 48mmol/mol or higher (LAB TESTING) (Type 2 diabetes is diagnosed in adults who are not pregnant and do not have haemoglobinopathy or haemolytic anaemia by a glycated haemoglobin (HbA1c) level of 48 mmol/mol or above.
The WHO state that diagnosis should be confirmed with a repeat HbA1c test, unless clinical symptoms and plasma glucose levels >11.1mmol/l are present in which case further testing is not required.)
FBG: >7.0mmol/L or higher x2
Dip urine to check for ketones
ASYMPTOMATIC
In the absence of symptoms – 2 abnormal results on separate days are required for the diagnosis.
Results:
- HbA1c > 48 mmol/l → repeat HbA1c test after 2 weeks → if HbA1c >48 mmol/l then code Diabetes and set recall
- HbA1c 42-47 mmol/l → code and set “at risk of diabetes” recall
May not be accurate in the following cases:
- ALL symptomatic children and young people
- Symptoms suggesting Type 1 diabetes/pancreatic insufficiency (any age)
- Short duration diabetes symptoms
- Patient at high risk of diabetes who are acutely ill
- Taking medication that may cause a rapid glucose rise e.g steroids, antipsychotics
- Acute pancreatic damage/pancreatic surgery
Patients with haemoglobinopathy – the labs test for this and will detect abnormalities.
A diagnosis of diabetes has important legal and medical implications for the patient and it is therefore essential to be secure in the diagnosis.
A diagnosis should never be made on the basis of glycosuria.
A stick reading of finger prick should be confirmed by a venous sample, as per NICE guidelines.
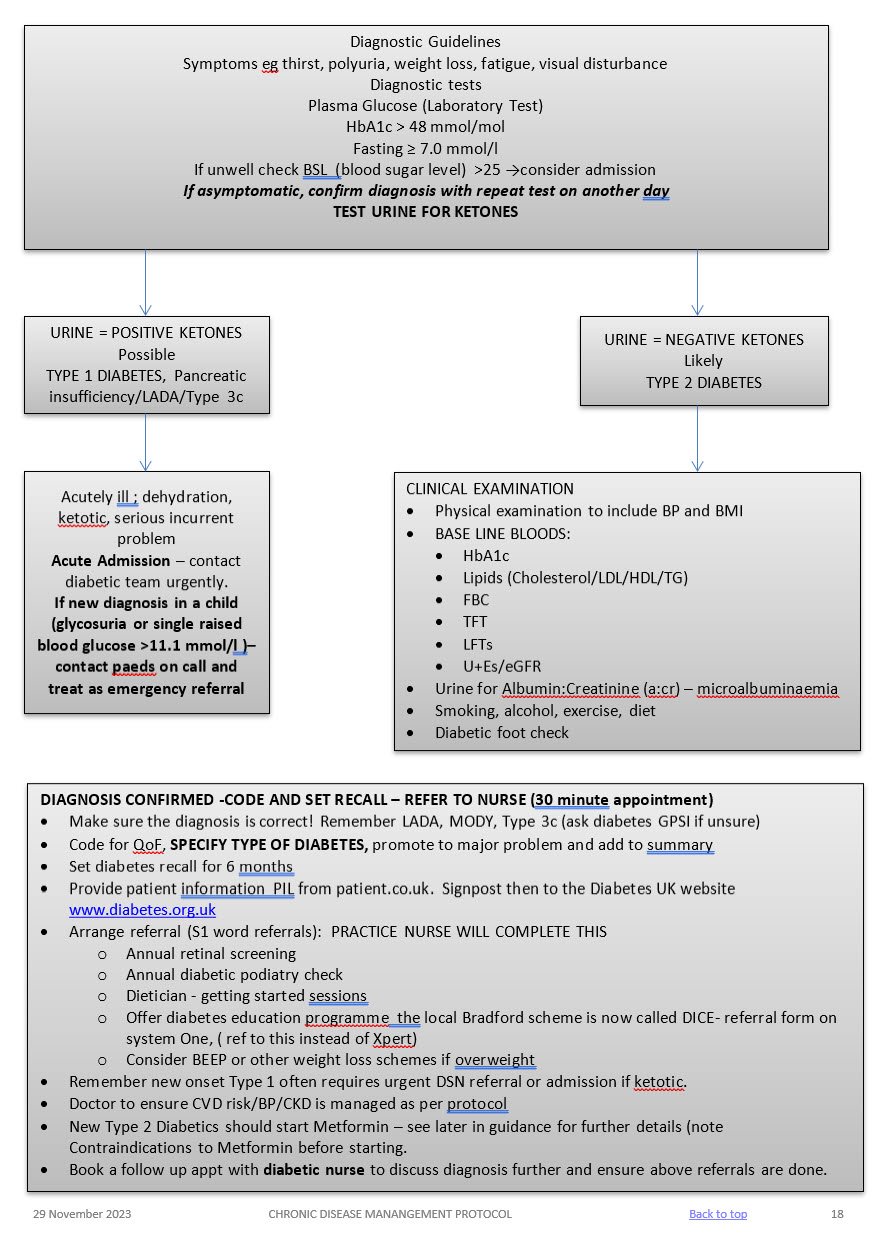
Admission
Admit to hospital if the person is at risk of a hyperglycaemic emergency (vomiting, abdominal pain reduced conscious level, heavy ketonuria, dehydration requiring IV fluids, hypotension, and serious intercurrent problem).
Same day referral
Refer to be seen on the same day if the patient is acutely ill, consider Type 1 Diabetes/pancreatic insufficiency if ketonuria present, the patient is slim and has a short history of marked symptoms (weight loss, thirst, and polyuria).
Early Referral
Diabetes and pregnancy requires referral to the hospital diabetes team
LIFESTYLE
BMI
Aim for healthy BMI <25 – consider dietition, Orlistat, other dietary measures & EXERCISE
ALCOHOL
Not to exceed recommended limits. (14 units men and women)
SMOKING
Stop!
BLOOD PRESSURE
Active management is essential!
Over half of all diabetics are hypertensive. Trials have shown that excellent BP control reduces retinopathy, nephropathy, strokes, heart failure and MI. BP control is as important as glycaemic control! TARGET < 130/80
Treatment
- 1st line – ACEi, ARB if they cannot tolerate it.
Ramipril starting regime derived from the HOPE study regime and BNF guidelines
If U&Es pre treatment reveal a creatinine < 150 micromol/l and a sodium >130 mmol/l then 2.5 mg Ramipril daily (1.25mg if on lower dose concomitant diuretics) for one week with check U&Es and an increase to 5.0 mg Ramipril for a further two weeks. Re-check U&Es and if indicated increase to 10mg Ramipril and repeat U&Es at least on an annual basis. If eGFR falls > 25% or creatinine rises by > 30% stop or back titrate treatment – see NICE guidelines. Don’t forget BNF cautions and contraindications. - 2nd line – CCB or, thiazide like diuretic or, Beta blocker (especially if there is a history of ischaemic heart disease),. Follow hypertension protocol
LIPIDS AND CVD RISK (see lipid modification protocol)
Offer generic Atorvastatin 40mg (Bradford Healthy Hearts) if their Q risk >10% (aged between 18-84 yrs), have been diabetic for > 10 years or, over 40 years old. Target chol <4mmol/l
For diabetics with established CVD offer secondary prevention or Chol > 4mmol/l – Atorvastatin 80mg
Triglycerides:
If TG level remains high (above 4.5mmol/l) please ref to CKS guidance on lipid modification or in-house lipid modification protocol.
Do not routinely offer Nicotinic acid or Omega fish oils.
MICROALBUMINURIA AND CKD
- All diabetics need testing annually for microalbuminuria and eGFR – microalbuminuria is the first sign of diabetic kidney disease and occurs before eGFR falls.
- SEE CKD PROTOCOL
ANTIPLATELETS
- Do not offer anti-platelets unless there is evidence of CVD
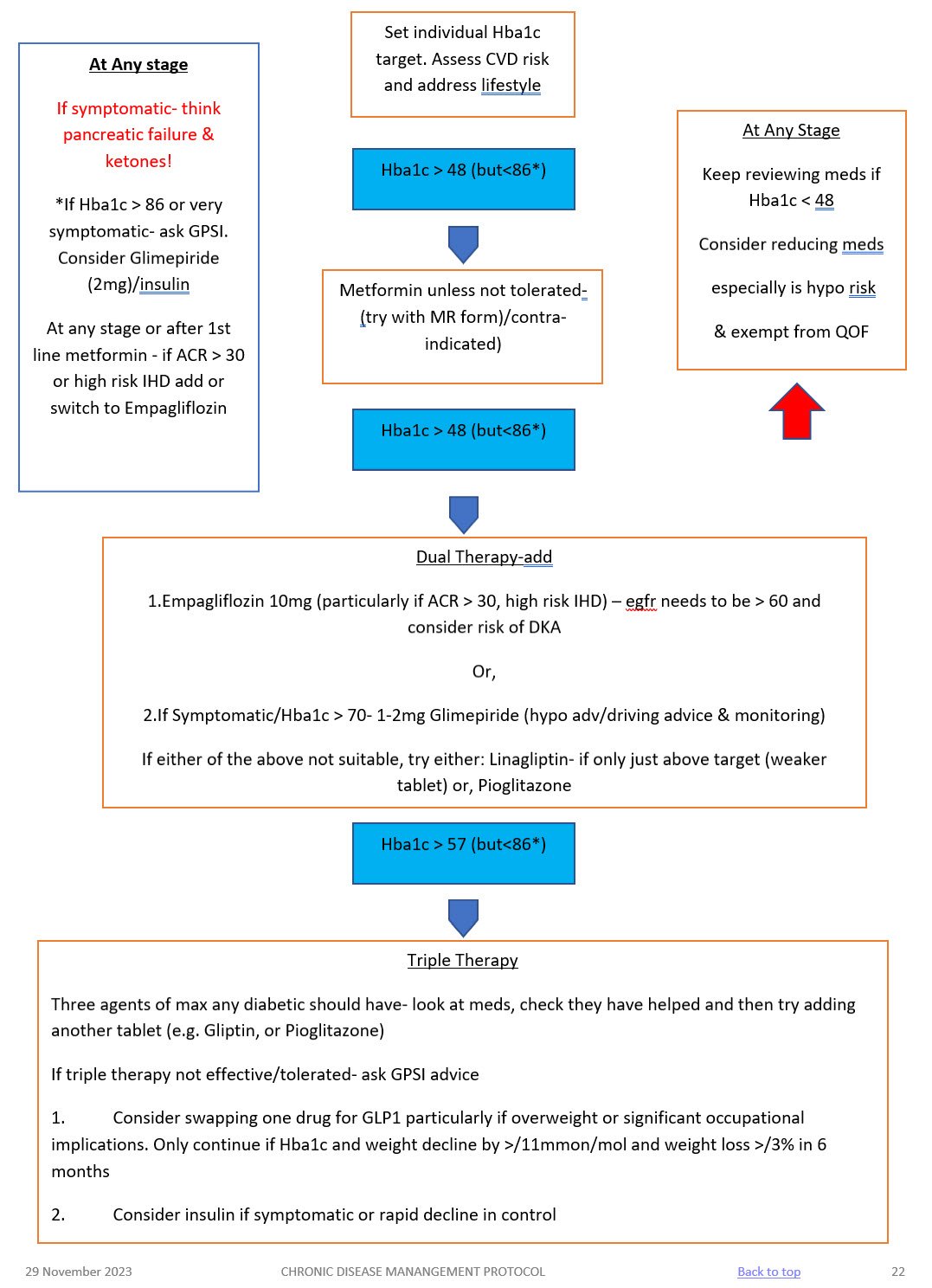
NICE recommended Hba1c targets are:
- 48mmol/mol – people who are managed by lifestyle and diet
- 48mmol/mol – people who are managed by lifestyle and diet combined with a single drug not associated with hypoglycaemia (such as metformin)
- 53mmol/mol – people who are taking a drug associated with hypoglycaemia (such as sulphonylurea), combination treatment
See table below for suggested targets for frail/elderly patients. Please exempt from QoF if you follow these targets putting an explanation in the notes.
Hba1c Target: aim for 48mmol/mol (if on diet or single drug not affected by hypoglycaemia ) or <53mmol/mol (if on SU, or more than one medication). Caution: elderly
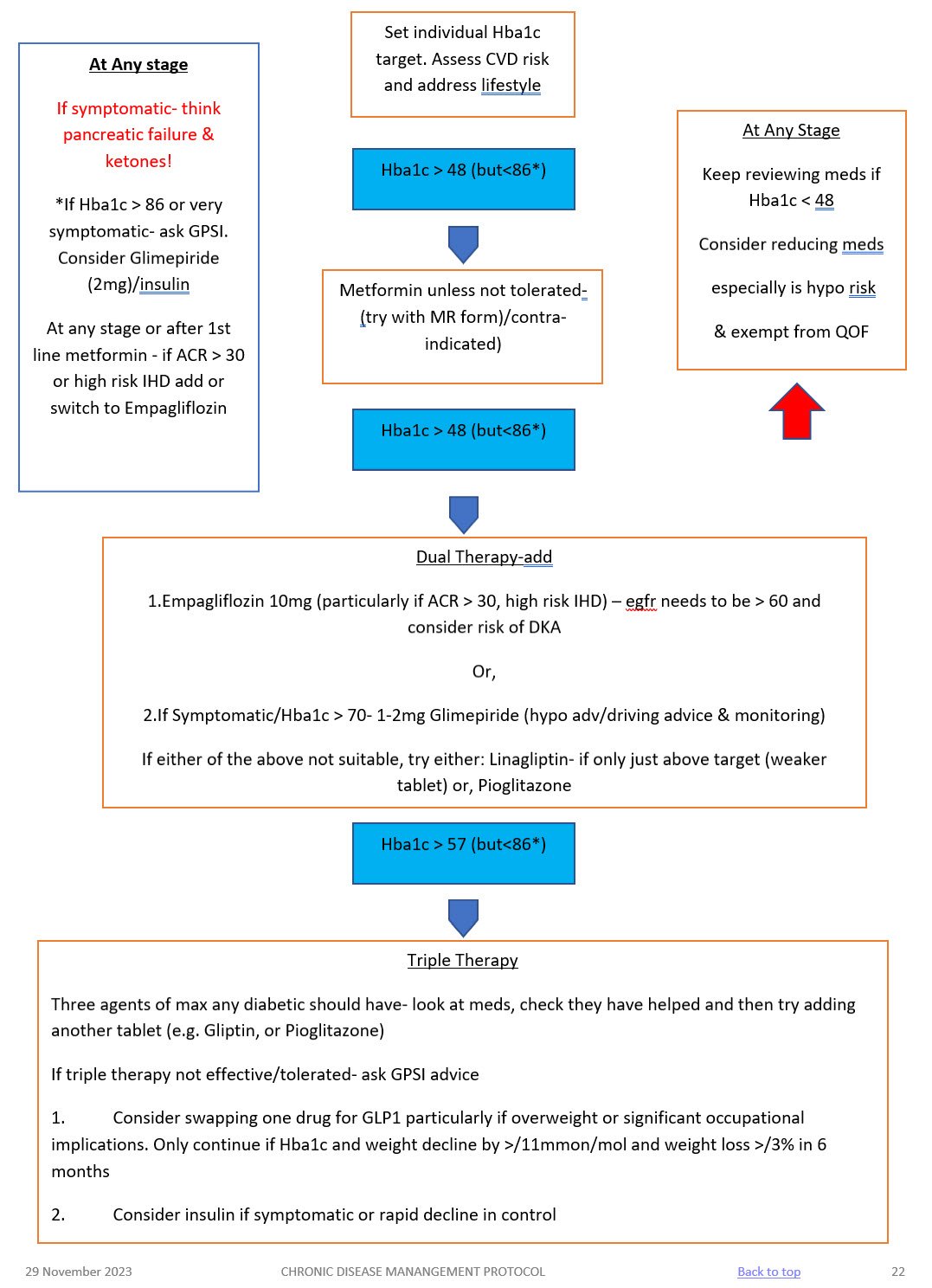
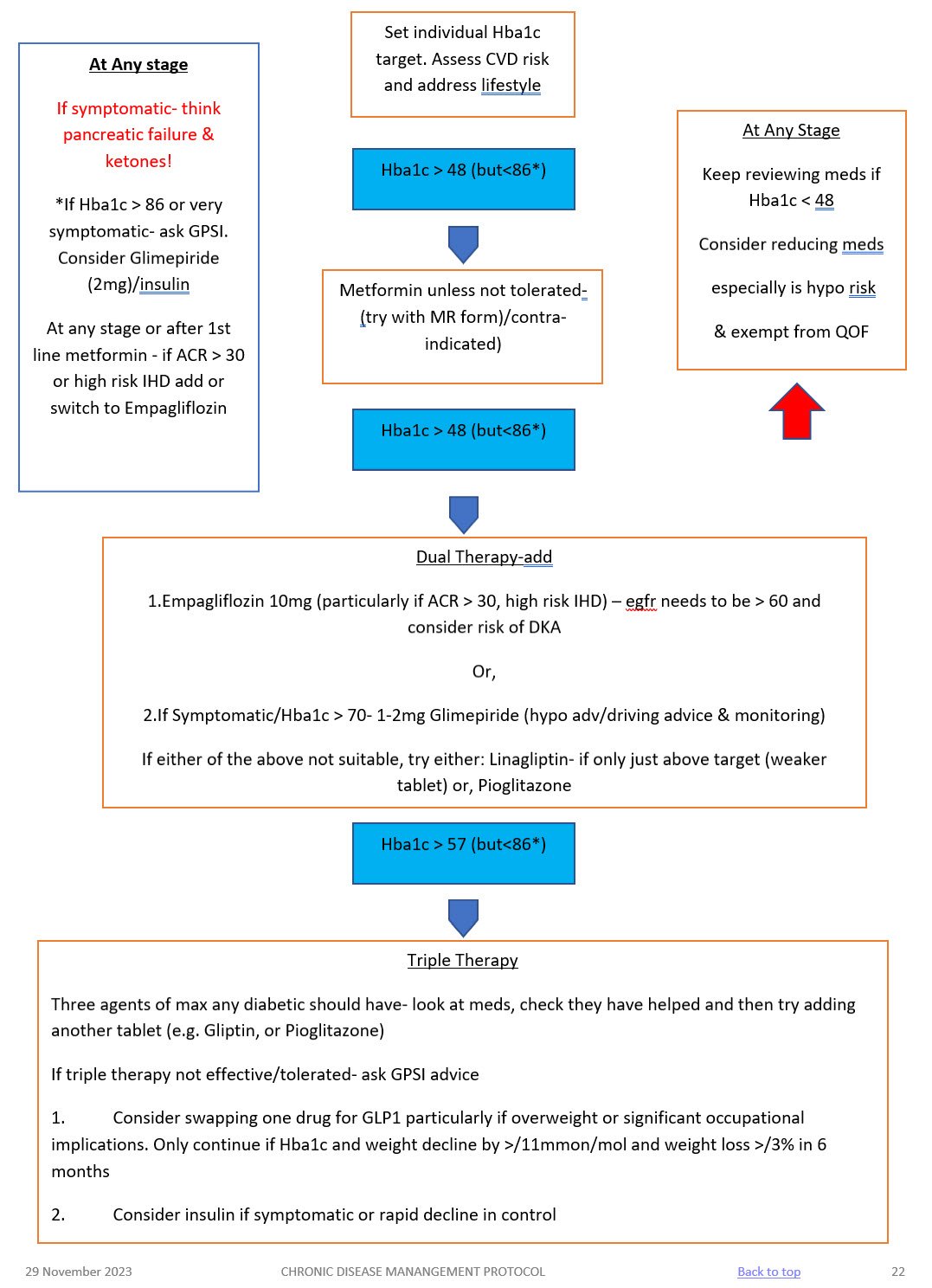
- Start Oral treatment usually Metformin at diagnosis. Metformin 500mg ideally with evening meal, increasing to 1 gram a week later if they have no side effects.
- Please remember Metformin is very effective, reduces cardiovascular risk, retards weight gain and is not usually associated with hypos – but is contra-indicated if Creatinine > 150 (or eGFR < 40) in CCF or significant hepatic dysfunction.
- Metformin has to be stopped if eGFR fall below 30!
- Metformin MR can be used if they run into problems with GI side effects.
- Don’t forget that on starting hypoglycaemics to complete the prescription exemption form for those patients under 60 years of age.
- If you are starting a sulphonylurea (ideally Glimepiride) – ensure they are counselled and documented about:
- symptoms of hypos
- hypo management
- hypos and driving and remind them about informing their car and travel insurer AND document this in their records. If they hold HGV or PSV license then check with the 6 monthly updated DVLA guidance with respect to them having to inform the DVLA.
- Ensure they have been given a glucometer and a sharps bin, test strips and lancets are added to their repeat prescription
- DISCUSS AKI SICK DAY RULES ADVICE – see hypertension protocol for full advice.
FUNCTIONALLY DEPENDENT
- Due to loss of function, having impairments of ADLs
- Increased likelihood of requiring addition medical &/or social care
- HBA1c target: 53 – 64mmol/mol
FRAIL
– Combination of significant fatigue, recent weight loss, severe restriction in mobility & strength, increased propensity for falls & increased risk of institutionalisation
– A recognised condition & accounts for 25% of older people with diabetes
– Clinical Frailty scale or CHSA 9-point scale (assessment tool)
– HBA1c target: 60-70mmol/mol
DEMENTIA
– Degree of cognitive impairment leading to sig. Memory problems, a degree of disorientation, or a change in personality & unable to self care
– MiniCog tool (easy to use assessment tool)
– HbA1c target: 60-70mmol/mol
END OF LIFE CARE
- Significant illness or malignancy & have life expectancy reduced to <1 year
- Glycaemic aim – hypo and symptomatic hyperglycaemia avoidance
Medication | Mode of action | Side effects | Cautions (check BNF for more detail) | Dose |
METFORMIN 1st line treatment, unless BMI <25 (23 in South Asian population) Low Hypo risk Reduces CVD risk, weight neutral | Helps to stop the liver producing new glucose. It helps to overcome insulin resistance by making insulin carry glucose into muscle cells more effectively.
| Main side effect if GI affects, generally dose dependent-can be reduced with gradual increase in dose over several weeks or trying modified release Metformin Also: metallic taste, reduced absorption of vitamin B12, build up of lactic acid in the blood, allergic reaction and liver problems. | STOP/DO NOT USE IF eGFR <30 ml/min *Lactic acidosis- care if eGFR < 45ml/min. Document that advice has been given to stop these tablets if they become dehydrated (restart when eating normally again) *GI side effects. Titrate dose slowly to reduce side effects NOTE IF ALT> 3 TIMES NORMAL | Start at 500mg ideally with evening meal, increasing to 1g with evening meal after a week if they have no side effects. Max dose 2 gram over 4 weeks. Consider slow release for to reduce tablet load or if they are struggling with GI side effects.
|
SGLT-inhibitor Empagliflozin Low hypo risk Can help with weight loss | Sodium-glucose co-transporter 2 (SGLT2) inhibitor that prevents glucose reuptake in the kidney, leading to the excretion of excess glucose in the urine. | Polyuria, polydipsia, thrush. UTI, fluid depletion Increased risk of amputation- avoid if h/o leg ulcers | Only start if Cr Clearance > 60. Care if > 75 years. Risk of postural hypotension. Care needed if they have skin ulcers – risk of amputation. Document advice about normoglycaemic ketoacidosis and give ketostix. | Empagliflozin 10mg. Can be increased to 25mg. Expensive so only continue if there is a clear response after 6 months |
SULPHONYLUREA (SU) Glimepiride Risk of hypos Good if rapid response is needed. | They work by stimulating cells in the pancreas to make more insulin. They also help insulin to work more effectively in the body.
| Weight gain. Hypoglycaemia, gastrointestinal side effects, low sodium, facial flushing and intolerance of alcohol, allergies etc.
| Can cause hypoglycaemia, particularly if there is renal impairment or they are elderly. Consider occupation – hypos if not eating regularly, fasting. Make sure you give and document advice about hypos. Make sure they are able to test their blood glucose – issue glucometer, test strips, lancets and sharps bin. (SGBM) Document advice about driving/insurance. | Start at 1mg and titrate up to 4mg depending on glucose level. Should have an effect on Hba1c over a 2 month period. |
GLIPTIN Do not cause weight gain and encourages patient satiety. Although they probably reduce Hba1c levels less than other drug treatments. Low hypo risk | They work by blocking the action of the enzyme, DPP-4, which destroys the hormone Incretin.
| Gastro-intestinal effects, oedema, headache, Avoid if h/o Pancreatitis or heart failure or liver problems. | *Expensive- only continue if they meet NICE guidance. *Not v powerful max likely reduction ~ 11 mmol/mol *Do not use if a h/o pancreatitis *Monitor egfr at reviews *Don’t use if heart failure risk | Linagliptin 5mg if eGFR < 50 |
GLITAZONE Pioglitazone Low hypo risk Consider in people with very significant features of metabolic syndrome. South Asian | Reducing insulin resistance. Improving insulin sensitivity.
| Oedema esp if heart failure or at risk. Rare reports of liver dysfunction. Weight gain, gastro-intestinal side effects, headache, dizziness.
| Discuss with member of Level 2 team before starting. Avoid if they have heart failure or risk of fluid overload Avoid if h/o bladder cancer, undiagnosed haematuria Avoid if fracture risk Monitor LFTs at each diabetic review. Annual urine dip looking for haematuria | Pioglitazone:15mg-30mg. A six month period may be needed to really see an effect from these tablets. NICE recommends that they are only continued if at least a 11 mmol/l reduction in Hba1c is seen within 6 months of starting the treatment.
|
GLP-1 mimetic/insulin | Discuss with Level 2 doctor |
|
- At first warning of episode of hypoglycaemia:
- Immediately treat with a 15-20g of a short-acting carbohydrate such as:
- 200 mls of Lucozade (please note Lucozade formula has changed so lower in sugar- need 200ml)
- 200mls of non-diet drink
- 4-5 glucose tablets
- 3-4 jelly babies
- 200mls of fruit juice
- Immediately treat with a 15-20g of a short-acting carbohydrate such as:
- If the hypo is more severe, and the patient cannot treat themselves:
- applying Glucagel (or treacle, jam or honey) on the inside of cheeks and gently massaging the outside of cheeks.
- if unconscious, Glucagon can be injected if the person treating has been trained to use it.
- Otherwise call an ambulance immediately
- Important:
- If unable to swallow or unconscious, do not give anything by mouth (including Glucagel, treacle, jam or honey). Make sure family and friends are aware of this. If unconscious, place patient in the recovery position (on side with head tilted back) so that tongue does not block throat.
- Follow-on treatment:
- To prevent blood glucose levels dropping again, follow sugary foods with 10-20g of a longer-acting carbohydrate such as:
- half a sandwich
- fruit
- a small bowl of cereal
- biscuits and milk
- the next meal if due
- Patients experiencing regular episodes of hypoglycaemia require prompt review by the diabetes team.
- Severe episodes of hypoglycaemia require urgent review by the diabetes team.
- To prevent blood glucose levels dropping again, follow sugary foods with 10-20g of a longer-acting carbohydrate such as:
Advise patients the following: if you do go down with a cold, flu or any other illness…
- The Basics
- Rest.
- Drink plenty of sugar-free fluids.
- Avoid too much caffeine as this could make you dehydrated.
- Take painkillers in the recommended doses as necessary.
- Contact your GP to see if treatment with antibiotics is necessary.
- If you are vomiting uncontrollably, contact your GP or diabetes clinic.
- Insulin or diabetes medications
- Keep taking your insulin or diabetes medications even if you are not eating. Stop metformin and blood pressure medication if you are dehydrated. CONSIDER AKI SICK DAY RULES – see hypertension protocol.
- Testing
- Test your blood or urine four or more times a day and night (ie at least eight times in a 24-hour period) and write the results down. If you are not well enough to do this, ask someone to do it for you.
- Ketoacidosis
- When diabetes is out of control as a result of severe sickness, it can lead to a condition called diabetic ketoacidosis or diabetic coma if you have Type 1 diabetes. The body produces high levels of ketone bodies causing too much acidity in the blood.
- Testing for ketones
- If you have Type 1 diabetes and your blood glucose level is 15 mmol/l or more or you have two per cent or more glucose in your urine, you will also need to test your urine or blood for ketones. They are a sign that your diabetes is seriously out of control. Ketones are especially likely when you are vomiting and can very quickly make you feel even worse. If a ketone test is positive, contact your GP or diabetes care team immediately.
- Food and drink
- It is important to keep taking your medication as normal and drink plenty of sugar-free drinks. Aim to drink at least three litres (five pints) a day. Try to keep to your normal meal pattern, but if you are unable to, for any reason, you can replace some or all of your meals with snacks and/or drinks that contain carbohydrate such as yoghurt, milk and other milky drinks, fruit juice or sugary drinks such as Lucozade, ordinary cola or lemonade. You may find it useful to let fizzy drinks go flat to help keep them down
Advise patients of the following:
- Vaccinations and/or malaria tablets
- Carry diabetes ID or a GP letter if carrying insulin and list of prescription drugs
- Carry all medication and blood glucose testing equipment in hand luggage
- Consider how to keep insulin cool if travelling for long periods
- Travel insurance: – Allow 2 weeks to buy travel insurance. – Don‟t just buy on price, check the cover and read the small print – – Be honest and declare all medical conditions
- Plan to take twice the quantity of medical supplies normally used
- Consider adjusting medication if travelling across time zones
- Consider adjustment to insulin if travelling to hot or cold climate
- Carry a European Health Insurance Card (EHIC) if travelling within Europe
www.ehic.org.uk, / 0845 605 0707
Consider availability of insulin if travelling abroad for long periods.
Interpreting blood results on pathology template – Remember frailty
- HbA1c <48 →select satisfactory→take no action – patient will be reviewed as per recall
- HbA1c 48-53 →select abnormal →speak to nurse → send task to admin to book tel appt with nurse to discuss abnormal result and document a suggested plan to up-titrate medication based on the above guidance for nurse to discuss with patient – nurse will discuss with patient possible changes to medication and then task Dr back to make changes and issue script. – if on single drug or diet only
- HbA1c <53 → select satisfactory →take no action – if on SU or combination drugs patient will attend at next review 6 months later
- HbA1c >53 → select abnormal (take into account patients age and fraility) →speak to nurse → send task to admin to book tel appt with nurse to discuss abnormal result and document a suggested plan to up-titrate medication based on the above guidance for nurse to discuss with patient – nurse will discuss with patient possible changes to medication and then task Dr back to make changes and issue script.
Any concerns – send message to Level 2 team
Using the SystmOne Template (CDM) for Diabetes.
See CDM review table
- Bloods: U&Es, eGFR, HbA1c, ALT (if first year on statin) and lipid profile – (Consider other tests if have other chronic diseases.)
- Urine ACR.
- BP
- Lifestyle discussion: smoking status/cessation advice, exercise status, alcohol intake, diet.
- BMI
- Retinal review.
- Foot check annually (in house) and record on the template. If moderate or high risk they need a referral to podiatry
- Any complications? erectile dysfunction, neuropathic pain, autonomic neuropathy.
- Hypo unawareness, ? hypos requiring external intervention (see DVLA guidelines).
- Review of blood monitoring – if they require monitoring.
- Medication review: concordance/indications/side effects/if on insulin – injection sites.
- Record medication review done, move date on till next review
- Assign diagnosis to repeat template medication.
- Add/move recall on. NB: Diabetics well be reviewed at least 6 monthly.
TARGETS AT A GLANCE
- BP: <130/80 – particularly if there are renal problems
- Get to non smoking: don’t forget smoking cessation
- Cholesterol: < 4.0mmol/l
- HbA1c:
- Diet alone or single drug not affected by hypoglycaemia <48mmol/l
- Medication <53mmol/l. Patient tailored care needed especially if they are elderly or there are concerns about hypogylcaemia.
- BMI: <25
Diabetes in pregnancy is associated with risks to the woman and the developing fetus.
Planning a pregnancy
Women planning a pregnancy should be referred to a diabetes pre-conception clinic.
Pre-pregnancy planning includes:
- Diet and exercise, weight loss advised if body mass index > 27kg/m2
- Retinal photography unless carried out in last 12months
- Renal assessment (including microalbuminuria)
- Folic acid 5mgs for 3 months preconception and continued for first trimester.
- Establish rubella status, booster organised if required.
- Blood pressure should be monitored
- Smoking/alcohol cessation advice
Review of medications
- Metformin may be used before and during pregnancy, as well as or instead of insulin. The diabetes antenatal clinic will oversee their care whilst pregnant.
- Isophane insulin is the first-choice long-acting insulin during pregnancy.
- Discontinue oral hypoglycaemic agents (apart from metformin), ACE-inhibitors, Angiotensin Receptor Blockers and statins
Gestational diabetes
- 6 weeks post-partum patients require a HbA1c to establish whether glucose tolerance has returned to normal.
- All patients require advice on their elevated long term risk of diabetes.
- All patients require advice on their risk of gestational diabetes in future pregnancies.
- All patients require advice regarding diet, weight control and exercise
All patients require an ANNUAL HbA1c in view of their elevated risk of Type 2 diabetes. Please add an ‘AT RISK OF DIABETES’ recall to their notes.
Urgencies & Emergencies
SYMPTOMATIC
Symptoms of hyperglycaemia (polyuria /polydipsia, unexplained weight loss. visual blurring, genital thrush, lethargy) plus either:
HbA1c: 48mmol/mol or higher (LAB TESTING) (Type 2 diabetes is diagnosed in adults who are not pregnant and do not have haemoglobinopathy or haemolytic anaemia by a glycated haemoglobin (HbA1c) level of 48 mmol/mol or above.
The WHO state that diagnosis should be confirmed with a repeat HbA1c test, unless clinical symptoms and plasma glucose levels >11.1mmol/l are present in which case further testing is not required.)
FBG: >7.0mmol/L or higher x2
Dip urine to check for ketones
ASYMPTOMATIC
In the absence of symptoms – 2 abnormal results on separate days are required for the diagnosis.
Results:
- HbA1c > 48 mmol/l → repeat HbA1c test after 2 weeks → if HbA1c >48 mmol/l then code Diabetes and set recall
- HbA1c 42-47 mmol/l → code and set “at risk of diabetes” recall
- FEEDING & FLUIDS: Ask about feeding / fluid intake and wet nappies (babies and infants can become dehydrated quickly). Red flag if not passed urine or wet nappy < 12hrs.
- PSYCHO-SOCIAL ENVIRONMENT: In chronic problems eg behavioural or chronic illness consider the psychological, social and environmental context – this will impact upon a child’s future health and development. Are there safeguarding issues / parental mental health issues, neglect, poverty and poor housing?
- LISTEN TO PARENTS: The carers or parents know their child best and their instinct is usually correct. LISTEN to their concerns.
- PMH & BH: Review the child’s past medical history and birth history as this gives clues to risk factors eg if premature or history of atopy may be more likely to have chronic respiratory problems. It may also inform parental developmental concerns eg. if slow to speak could this be due to ear infections?
- FEEDING & FLUIDS: Ask about feeding / fluid intake and wet nappies (babies and infants can become dehydrated quickly). Red flag if not passed urine or wet nappy < 12hrs.
- PSYCHO-SOCIAL ENVIRONMENT: In chronic problems eg behavioural or chronic illness consider the psychological, social and environmental context – this will impact upon a child’s future health and development. Are there safeguarding issues / parental mental health issues, neglect, poverty and poor housing?
Admission
Admit to hospital if the person is at risk of a hyperglycaemic emergency (vomiting, abdominal pain reduced conscious level, heavy ketonuria, dehydration requiring IV fluids, hypotension, and serious intercurrent problem).
Same day referral
Refer to be seen on the same day if the patient is acutely ill, consider Type 1 Diabetes/pancreatic insufficiency if ketonuria present, the patient is slim and has a short history of marked symptoms (weight loss, thirst, and polyuria).
Early Referral
Diabetes and pregnancy requires referral to the hospital diabetes team
LIFESTYLE
BMI
Aim for healthy BMI <25 – consider dietition, Orlistat, other dietary measures & EXERCISE
ALCOHOL
Not to exceed recommended limits. (14 units men and women)
SMOKING
Stop!
BLOOD PRESSURE
Active management is essential!
Over half of all diabetics are hypertensive. Trials have shown that excellent BP control reduces retinopathy, nephropathy, strokes, heart failure and MI. BP control is as important as glycaemic control! TARGET < 130/80
Treatment
- 1st line – ACEi, ARB if they cannot tolerate it.
Ramipril starting regime derived from the HOPE study regime and BNF guidelines
If U&Es pre treatment reveal a creatinine < 150 micromol/l and a sodium >130 mmol/l then 2.5 mg Ramipril daily (1.25mg if on lower dose concomitant diuretics) for one week with check U&Es and an increase to 5.0 mg Ramipril for a further two weeks. Re-check U&Es and if indicated increase to 10mg Ramipril and repeat U&Es at least on an annual basis. If eGFR falls > 25% or creatinine rises by > 30% stop or back titrate treatment – see NICE guidelines. Don’t forget BNF cautions and contraindications. - 2nd line – CCB or, thiazide like diuretic or, Beta blocker (especially if there is a history of ischaemic heart disease),. Follow hypertension protocol
LIPIDS AND CVD RISK (see lipid modification protocol)
Offer generic Atorvastatin 40mg (Bradford Healthy Hearts) if their Q risk >10% (aged between 18-84 yrs), have been diabetic for > 10 years or, over 40 years old. Target chol <4mmol/l
For diabetics with established CVD offer secondary prevention or Chol > 4mmol/l – Atorvastatin 80mg
Triglycerides:
If TG level remains high (above 4.5mmol/l) please ref to CKS guidance on lipid modification or in-house lipid modification protocol.
Do not routinely offer Nicotinic acid or Omega fish oils.
MICROALBUMINURIA AND CKD
- All diabetics need testing annually for microalbuminuria and eGFR – microalbuminuria is the first sign of diabetic kidney disease and occurs before eGFR falls.
- SEE CKD PROTOCOL
ANTIPLATELETS
- Do not offer anti-platelets unless there is evidence of CVD
NICE recommended Hba1c targets are:
- 48mmol/mol – people who are managed by lifestyle and diet
- 48mmol/mol – people who are managed by lifestyle and diet combined with a single drug not associated with hypoglycaemia (such as metformin)
- 53mmol/mol – people who are taking a drug associated with hypoglycaemia (such as sulphonylurea), combination treatment
See table below for suggested targets for frail/elderly patients. Please exempt from QoF if you follow these targets putting an explanation in the notes.
Hba1c Target: aim for 48mmol/mol (if on diet or single drug not affected by hypoglycaemia ) or <53mmol/mol (if on SU, or more than one medication). Caution: elderly
- Start Oral treatment usually Metformin at diagnosis. Metformin 500mg ideally with evening meal, increasing to 1 gram a week later if they have no side effects.
- Please remember Metformin is very effective, reduces cardiovascular risk, retards weight gain and is not usually associated with hypos – but is contra-indicated if Creatinine > 150 (or eGFR < 40) in CCF or significant hepatic dysfunction.
- Metformin has to be stopped if eGFR fall below 30!
- Metformin MR can be used if they run into problems with GI side effects.
- Don’t forget that on starting hypoglycaemics to complete the prescription exemption form for those patients under 60 years of age.
- If you are starting a sulphonylurea (ideally Glimepiride) – ensure they are counselled and documented about:
- symptoms of hypos
- hypo management
- hypos and driving and remind them about informing their car and travel insurer AND document this in their records. If they hold HGV or PSV license then check with the 6 monthly updated DVLA guidance with respect to them having to inform the DVLA.
- Ensure they have been given a glucometer and a sharps bin, test strips and lancets are added to their repeat prescription
- DISCUSS AKI SICK DAY RULES ADVICE – see hypertension protocol for full advice.
FUNCTIONALLY DEPENDENT
- Due to loss of function, having impairments of ADLs
- Increased likelihood of requiring addition medical &/or social care
- HBA1c target: 53 – 64mmol/mol
FRAIL
– Combination of significant fatigue, recent weight loss, severe restriction in mobility & strength, increased propensity for falls & increased risk of institutionalisation
– A recognised condition & accounts for 25% of older people with diabetes
– Clinical Frailty scale or CHSA 9-point scale (assessment tool)
– HBA1c target: 60-70mmol/mol
DEMENTIA
– Degree of cognitive impairment leading to sig. Memory problems, a degree of disorientation, or a change in personality & unable to self care
– MiniCog tool (easy to use assessment tool)
– HbA1c target: 60-70mmol/mol
END OF LIFE CARE
- Significant illness or malignancy & have life expectancy reduced to <1 year
- Glycaemic aim – hypo and symptomatic hyperglycaemia avoidance
Medication | Mode of action | Side effects | Cautions (check BNF for more detail) | Dose |
METFORMIN 1st line treatment, unless BMI <25 (23 in South Asian population) Low Hypo risk Reduces CVD risk, weight neutral | Helps to stop the liver producing new glucose. It helps to overcome insulin resistance by making insulin carry glucose into muscle cells more effectively.
| Main side effect if GI affects, generally dose dependent-can be reduced with gradual increase in dose over several weeks or trying modified release Metformin Also: metallic taste, reduced absorption of vitamin B12, build up of lactic acid in the blood, allergic reaction and liver problems. | STOP/DO NOT USE IF eGFR <30 ml/min *Lactic acidosis- care if eGFR < 45ml/min. Document that advice has been given to stop these tablets if they become dehydrated (restart when eating normally again) *GI side effects. Titrate dose slowly to reduce side effects NOTE IF ALT> 3 TIMES NORMAL | Start at 500mg ideally with evening meal, increasing to 1g with evening meal after a week if they have no side effects. Max dose 2 gram over 4 weeks. Consider slow release for to reduce tablet load or if they are struggling with GI side effects.
|
SGLT-inhibitor Empagliflozin Low hypo risk Can help with weight loss | Sodium-glucose co-transporter 2 (SGLT2) inhibitor that prevents glucose reuptake in the kidney, leading to the excretion of excess glucose in the urine. | Polyuria, polydipsia, thrush. UTI, fluid depletion Increased risk of amputation- avoid if h/o leg ulcers | Only start if Cr Clearance > 60. Care if > 75 years. Risk of postural hypotension. Care needed if they have skin ulcers – risk of amputation. Document advice about normoglycaemic ketoacidosis and give ketostix. | Empagliflozin 10mg. Can be increased to 25mg. Expensive so only continue if there is a clear response after 6 months |
SULPHONYLUREA (SU) Glimepiride Risk of hypos Good if rapid response is needed. | They work by stimulating cells in the pancreas to make more insulin. They also help insulin to work more effectively in the body.
| Weight gain. Hypoglycaemia, gastrointestinal side effects, low sodium, facial flushing and intolerance of alcohol, allergies etc.
| Can cause hypoglycaemia, particularly if there is renal impairment or they are elderly. Consider occupation – hypos if not eating regularly, fasting. Make sure you give and document advice about hypos. Make sure they are able to test their blood glucose – issue glucometer, test strips, lancets and sharps bin. (SGBM) Document advice about driving/insurance. | Start at 1mg and titrate up to 4mg depending on glucose level. Should have an effect on Hba1c over a 2 month period. |
GLIPTIN Do not cause weight gain and encourages patient satiety. Although they probably reduce Hba1c levels less than other drug treatments. Low hypo risk | They work by blocking the action of the enzyme, DPP-4, which destroys the hormone Incretin.
| Gastro-intestinal effects, oedema, headache, Avoid if h/o Pancreatitis or heart failure or liver problems. | *Expensive- only continue if they meet NICE guidance. *Not v powerful max likely reduction ~ 11 mmol/mol *Do not use if a h/o pancreatitis *Monitor egfr at reviews *Don’t use if heart failure risk | Linagliptin 5mg if eGFR < 50 |
GLITAZONE Pioglitazone Low hypo risk Consider in people with very significant features of metabolic syndrome. South Asian | Reducing insulin resistance. Improving insulin sensitivity.
| Oedema esp if heart failure or at risk. Rare reports of liver dysfunction. Weight gain, gastro-intestinal side effects, headache, dizziness.
| Discuss with member of Level 2 team before starting. Avoid if they have heart failure or risk of fluid overload Avoid if h/o bladder cancer, undiagnosed haematuria Avoid if fracture risk Monitor LFTs at each diabetic review. Annual urine dip looking for haematuria | Pioglitazone:15mg-30mg. A six month period may be needed to really see an effect from these tablets. NICE recommends that they are only continued if at least a 11 mmol/l reduction in Hba1c is seen within 6 months of starting the treatment.
|
GLP-1 mimetic/insulin | Discuss with Level 2 doctor |
|
- At first warning of episode of hypoglycaemia:
- Immediately treat with a 15-20g of a short-acting carbohydrate such as:
- 200 mls of Lucozade (please note Lucozade formula has changed so lower in sugar- need 200ml)
- 200mls of non-diet drink
- 4-5 glucose tablets
- 3-4 jelly babies
- 200mls of fruit juice
- Immediately treat with a 15-20g of a short-acting carbohydrate such as:
- If the hypo is more severe, and the patient cannot treat themselves:
- applying Glucagel (or treacle, jam or honey) on the inside of cheeks and gently massaging the outside of cheeks.
- if unconscious, Glucagon can be injected if the person treating has been trained to use it.
- Otherwise call an ambulance immediately
- Important:
- If unable to swallow or unconscious, do not give anything by mouth (including Glucagel, treacle, jam or honey). Make sure family and friends are aware of this. If unconscious, place patient in the recovery position (on side with head tilted back) so that tongue does not block throat.
- Follow-on treatment:
- To prevent blood glucose levels dropping again, follow sugary foods with 10-20g of a longer-acting carbohydrate such as:
- half a sandwich
- fruit
- a small bowl of cereal
- biscuits and milk
- the next meal if due
- Patients experiencing regular episodes of hypoglycaemia require prompt review by the diabetes team.
- Severe episodes of hypoglycaemia require urgent review by the diabetes team.
- To prevent blood glucose levels dropping again, follow sugary foods with 10-20g of a longer-acting carbohydrate such as:
Advise patients the following: if you do go down with a cold, flu or any other illness…
- The Basics
- Rest.
- Drink plenty of sugar-free fluids.
- Avoid too much caffeine as this could make you dehydrated.
- Take painkillers in the recommended doses as necessary.
- Contact your GP to see if treatment with antibiotics is necessary.
- If you are vomiting uncontrollably, contact your GP or diabetes clinic.
- Insulin or diabetes medications
- Keep taking your insulin or diabetes medications even if you are not eating. Stop metformin and blood pressure medication if you are dehydrated. CONSIDER AKI SICK DAY RULES – see hypertension protocol.
- Testing
- Test your blood or urine four or more times a day and night (ie at least eight times in a 24-hour period) and write the results down. If you are not well enough to do this, ask someone to do it for you.
- Ketoacidosis
- When diabetes is out of control as a result of severe sickness, it can lead to a condition called diabetic ketoacidosis or diabetic coma if you have Type 1 diabetes. The body produces high levels of ketone bodies causing too much acidity in the blood.
- Testing for ketones
- If you have Type 1 diabetes and your blood glucose level is 15 mmol/l or more or you have two per cent or more glucose in your urine, you will also need to test your urine or blood for ketones. They are a sign that your diabetes is seriously out of control. Ketones are especially likely when you are vomiting and can very quickly make you feel even worse. If a ketone test is positive, contact your GP or diabetes care team immediately.
- Food and drink
- It is important to keep taking your medication as normal and drink plenty of sugar-free drinks. Aim to drink at least three litres (five pints) a day. Try to keep to your normal meal pattern, but if you are unable to, for any reason, you can replace some or all of your meals with snacks and/or drinks that contain carbohydrate such as yoghurt, milk and other milky drinks, fruit juice or sugary drinks such as Lucozade, ordinary cola or lemonade. You may find it useful to let fizzy drinks go flat to help keep them down
Advise patients of the following:
- Vaccinations and/or malaria tablets
- Carry diabetes ID or a GP letter if carrying insulin and list of prescription drugs
- Carry all medication and blood glucose testing equipment in hand luggage
- Consider how to keep insulin cool if travelling for long periods
- Travel insurance: – Allow 2 weeks to buy travel insurance. – Don‟t just buy on price, check the cover and read the small print – – Be honest and declare all medical conditions
- Plan to take twice the quantity of medical supplies normally used
- Consider adjusting medication if travelling across time zones
- Consider adjustment to insulin if travelling to hot or cold climate
- Carry a European Health Insurance Card (EHIC) if travelling within Europe
www.ehic.org.uk, / 0845 605 0707
Consider availability of insulin if travelling abroad for long periods.
Interpreting blood results on pathology template – Remember frailty
- HbA1c <48 →select satisfactory→take no action – patient will be reviewed as per recall
- HbA1c 48-53 →select abnormal →speak to nurse → send task to admin to book tel appt with nurse to discuss abnormal result and document a suggested plan to up-titrate medication based on the above guidance for nurse to discuss with patient – nurse will discuss with patient possible changes to medication and then task Dr back to make changes and issue script. – if on single drug or diet only
- HbA1c <53 → select satisfactory →take no action – if on SU or combination drugs patient will attend at next review 6 months later
- HbA1c >53 → select abnormal (take into account patients age and fraility) →speak to nurse → send task to admin to book tel appt with nurse to discuss abnormal result and document a suggested plan to up-titrate medication based on the above guidance for nurse to discuss with patient – nurse will discuss with patient possible changes to medication and then task Dr back to make changes and issue script.
Any concerns – send message to Level 2 team
Using the SystmOne Template (CDM) for Diabetes.
See CDM review table
- Bloods: U&Es, eGFR, HbA1c, ALT (if first year on statin) and lipid profile – (Consider other tests if have other chronic diseases.)
- Urine ACR.
- BP
- Lifestyle discussion: smoking status/cessation advice, exercise status, alcohol intake, diet.
- BMI
- Retinal review.
- Foot check annually (in house) and record on the template. If moderate or high risk they need a referral to podiatry
- Any complications? erectile dysfunction, neuropathic pain, autonomic neuropathy.
- Hypo unawareness, ? hypos requiring external intervention (see DVLA guidelines).
- Review of blood monitoring – if they require monitoring.
- Medication review: concordance/indications/side effects/if on insulin – injection sites.
- Record medication review done, move date on till next review
- Assign diagnosis to repeat template medication.
- Add/move recall on. NB: Diabetics well be reviewed at least 6 monthly.
TARGETS AT A GLANCE
- BP: <130/80 – particularly if there are renal problems
- Get to non smoking: don’t forget smoking cessation
- Cholesterol: < 4.0mmol/l
- HbA1c:
- Diet alone or single drug not affected by hypoglycaemia <48mmol/l
- Medication <53mmol/l. Patient tailored care needed especially if they are elderly or there are concerns about hypogylcaemia.
- BMI: <25
Diabetes in pregnancy is associated with risks to the woman and the developing fetus.
Planning a pregnancy
Women planning a pregnancy should be referred to a diabetes pre-conception clinic.
Pre-pregnancy planning includes:
- Diet and exercise, weight loss advised if body mass index > 27kg/m2
- Retinal photography unless carried out in last 12months
- Renal assessment (including microalbuminuria)
- Folic acid 5mgs for 3 months preconception and continued for first trimester.
- Establish rubella status, booster organised if required.
- Blood pressure should be monitored
- Smoking/alcohol cessation advice
Review of medications
- Metformin may be used before and during pregnancy, as well as or instead of insulin. The diabetes antenatal clinic will oversee their care whilst pregnant.
- Isophane insulin is the first-choice long-acting insulin during pregnancy.
- Discontinue oral hypoglycaemic agents (apart from metformin), ACE-inhibitors, Angiotensin Receptor Blockers and statins
Gestational diabetes
- 6 weeks post-partum patients require a HbA1c to establish whether glucose tolerance has returned to normal.
- All patients require advice on their elevated long term risk of diabetes.
- All patients require advice on their risk of gestational diabetes in future pregnancies.
- All patients require advice regarding diet, weight control and exercise
All patients require an ANNUAL HbA1c in view of their elevated risk of Type 2 diabetes. Please add an ‘AT RISK OF DIABETES’ recall to their notes.

Bradford VTS Online Resources:
Clinical Knowledge:
Paediatrics (Infants & Children) by Dr Jenny Wright (Bradford), Aug 2021
Abdominal Pain
Abdominal pain is commonly due to a virus and in infants, colic. Most of you will think about constipation, UTI, appendicitis (rare in v. young children, but still possible). But a lot of you will forget to exclude lower lobe pneumonia and testicular torsion. Also don’t forget about 1st presentation of DKA (e.g. lethargic child with abdo pain – check urine for glucose and ketones). And of course intussusception. Look for these – don’t be fooled into making a mistake because of availability bias.
Availability bias (also known as availability heuristic) = the human tendency to rely on information that comes readily to mind when evaluating situations or making decisions. (PS Heuristic is a fancy word for a mental shortcut that helps avoid cognitive overload e.g. when you see a person with their hood up in a dark alley – you automatically decide to walk a bit faster).
Some Helpful Pointers
- Colic – this should be a diagnosis of exclusion. Colic really isn’t a diagnosis because is has no pathological basis for it – we don’t know what it is! Have you heard of the 3x3x3 infantile colic rule – don’t worry if you haven’t because IT IS NON-SENSE (this stupid illogical old rule says that infantile colic is where an infant cries for more than 3 hours a day, 3 days per week and for longer than 3 weeks. BUT IT IS NONSENSE). So how do you tell? Do a thorough assessment. If you can then be fairly sure there is no other course (like the things below) AND there are no alarm features, then it may be due to colic. No one truly knows what colic is be we think that it is due to sensations in the infants bowel (i.e. they are getting used to peristalsis). There are no effective treatments for colic. Parents must know that if all the infants needs have been met (feeding, clothed, physical comfort & love) and there are no alarm features (like a rash, not drinking, not passing urine, reduced social interaction/periods of contentment inbetween), then it is OK to allow them to cry.
- Mesenteric Adenitis – is common. Where the mesenteric lymph nodes become inflamed as a result of a viral intestinal infection, or even an viral upper respiratory tract infection. They can even have localised abdominal tenderness – BUT – if there are red flag signs or symptoms you should still take these seriously
- Gastroenteritis – more likely is vomiting precedes abdominal pain. Diarrhoea is also strong indicator of viral gastroenteritis. But always exclude a surgical cause like intusussception and appendicitis. Feel the belly, do the vitals.
- Non-IgE food allergy – can cause acute abdominal pain. HOWEVER, diagnosis best not made acutely. Take a good history + a food diary + follow-up will help you decide if this is an appropriate diagnosis.
- Constipation – common cause acute abdominal pain in children. Remember, the child will be AFEBRILE – no fever! There are two main pitfalls. The first is to miss the diagnosis because the child or parent doesn’t think the child is constipated. The second is to think that because the presentation is acute, the problem just needs a brief period of treatment. If they are constipated enough to present with acute pain, the problem is chronic and should be treated as such as per NICE guidelines.
- Urinary Tract Infection – Abdominal pain +/- vomiting is a common way for children to present with UTI, but remember, there should be no diarrhoea if you are considering this diagnosis.
- Pregnancy – don’t forget this possibility in children (common pitfall). In a 12 year old and above, think ectopic pregnancy as a possiblity. Do a pregnancy test.
Emergencies
- Appendicitis – Uncommon in infants and small children under age 5 – but not so rare that you won’t see a case every now and then – so be mindful – reassess if needs be or safety-net. Appendicitis usually affects 5-20 year olds.
- Testicular torsion – Boys with abdo pain – always examine the genitals. Do it, even if the last 100 times were normal, it only takes a few seconds, yet might save a life.
- Intussusception – Rare but deadly. Episodes of pallor and signs of being significantly unwell are reasons to suspect intussusception. Bloody and mucousy (redcurrent jelly-like) stools make it easier to diagnose but may be a late sign.
- Diabetic Ketoacidosis – often missed. If a bit more lethargic than your typical gastroenteritis case, or if there is a report of polyuria, think DKA. Dip the urine for ketone & glucose.
Emergencies - meningitis, acute asthma, anaphylaxis & DKA
Meningococcal sepsis and Meningitis (90% occur <5yrs)
- NON blanching petechial rash or purpura in unwell child = sepsis until proven otherwise call 999 and administer Benzylpenicillin or ceftriaxime IV or IM.
- Also if irritable, poor feeding, respiratory distress, mottled skin, fever (not always seen in neonates), seizures, vomiting, headaches, photophobia, altered consciousness call 999 and if time give IM benzylpenicillin.
Withhold benzylpenicillin only in children who have a clear history of anaphylaxis after a previous dose of penicillin; a history of a rash following penicillin is not a contraindication
Recommended doses
- in adults and children of 10 years or more : IV or IM benzylpenicillin 1.2 g
- for children 1 to 9 years : IV or IM benzylpenicillin 600 mg
- for children less than 1 year : IV or IM benzylpenicillin 300 mg
Acute Asthma in >1yr old
Ref. Management of acute asthma in children aged 1 year and over (2019 BTS / SIGN)
- Severe call 999 If SpO2 <92% place on high flow oxygen via nebuliser with salbutamol 2.5-5mg +/- ipratropium (useful especially if <2yrs).
- Admit children whose SpO2 <94% and those who are too exhausted to speak or feed. Consider admission where RR >40/min in 1-5yrs or >30/min >5yrs or where PEFR is <50% of their best. Also where recessing or using accessory muscles to breath.
- If mild to moderate symptoms and sats >94% advise up to ten puffs via spacer every 3-4hrs and advise parents/carers of children with acute asthma at home and symptoms not controlled by up to 10 puffs of salbutamol, to seek urgent medical attention.
- Aim to review within 2 days and give oral steroids early in the treatment of acute asthma. Use a dose of 10 mg prednisolone for children under 2 years of age, 20 mg for children aged 2-5 years and 30-40 mg for children >5 years (between 1-2mg / kg generally). Usually 3-5 days.
Anaphylaxis
An outline anaphylaxis treatment algorithm for children for medical first responders is presented below
- consider anaphylaxis when compatible history of severe allergic-type reaction with respiratory difficulty and/or hypotension especially if skin changes present. Give oxygen and call 999
- assess for signs of stridor, wheeze, respiratory distress or clinical signs of shock.
- give adrenaline (epinephrine) 1:1000 solution. Dose is dependent on age and size of child
- > 12 years: 500 micrograms IM (0.5 mL) i.e. same as adult dose
- > 6 – 12 years: 300 micrograms IM (0.3 mL)
- > 6 months – 6 years: 150 micrograms IM (0.15 mL)
- < 6 months: 150 micrograms IM (0.15 mL)
- the adrenaline dose is repeated in 5 minutes if no clinical improvement and give an antihistamine (chlorphenamine)
- >12 years: 10-20 mg IM
- 6-12 years: 5-10 mg IM
- 1-6 years: 2.5-5 mg IM
- in addition for all severe or recurrent reactions and patients with asthma give hydrocortisone
- >12 years: 100-500 mg IM or slow IV
- 6-12 years: 100 mg IM or slow IV
- 1-6 years: 50 mg IM or slow IV
Emergency treatment of anaphylactic reactions. Guidelines for healthcare providers. Working Group of the Resuscitation Council (UK).2008 Last reviewed 01/2018
New Type I Diabetes and Diabetic Ketoacidosis
- Consider Type I diabetes in child with subacute weight loss, fatigue, thirst, polyuria and lassitude – check urine for glucose and ketones then BM if positive – Type I DM – ADMIT
- If DKA usually very unwell as illness precipitates this, with vomiting, ketotic breath and shocked – ADMIT VIA 999
Same-day Referral to Paeds
- Bronchiolitis – <1yr due to RSV admit if poor feeding, recessing or unwell
- Dehydration due to vomiting/diarrhoea – urine output poor (dry nappies over 12hrs) / no tears / sunken anterior fontanelle or reduced capillary refill time.
- ENT – Quinsy or mastoiditis (tender mastoid unwell with otitis media),
- Febrile convulsion or first fit admit for investigation (give oxygen and ring 999)
- Fever of unknown origin in especially if sustained >5 days or in baby <3mnths or unwell <12mnth – consider admission will need needs a septic screen. This can often be urinary sepsis (see NICE 2019 Fever in children <5yrs).
- Head Injury –with any loss of consciousness, recurrent vomiting, confusion, neurology or significant mechanism – admit (see NICE guidelines on head injury 2014).
- Henoch Schonlein Purpura – needs BP, UES and urine dip so admit and will need follow up urine dips for several weeks (according to local protocol)
- Kawasakis – sustained high temp for >5 days, dry lips and mouth, flaking desquamation and oedema of fingers and toes, bilateral conjunctivitis, cervical LN. Admit as common complications of coronary arteritis and aneurysm.
- Non-Accidental Injury eg bruising in the non-mobile child -think safeguarding and admit for examination (check local safeguarding pathways).
- Surgical
- appendicitis (can they jump or cough without pain in RIF?) If not admit.
- Testicular pain swollen high tender testicle – torsion.
- Pyloric stenosis (failure to thrive, projectile vomiting and unwell/ dehydrated) presents between 2-6wks.
- Inguinal hernias in neonate
- Transient Synovitis Unable to weight bear / acutely atraumatic immobility = irritable hip (transient synovitis) or Perthes – admit.
DON’T FORGET: NICE traffic light system <5yrs useful to assess the sick child and guide admission